Building trust together: How community led research is changing the approach to clinical trials
For people with blood cancer clinical trials take on added significance, as most can't be treated with surgery or radiotherapy. For some people, participating in a trial will be their best and only treatment option.

Research has shown that some types of blood cancer occur more often in certain ethnic groups. Despite this, there is evidence to suggest people from minority ethnic communities are less likely to be recruited to trials. Yet how the disease presents itself and the person’s response to treatment can vary by factors like ethnicity, for example, members of the black community with myeloma are often diagnosed at a younger age and with more advanced disease, leading to gaps in knowledge and care, and in some cases outcomes.
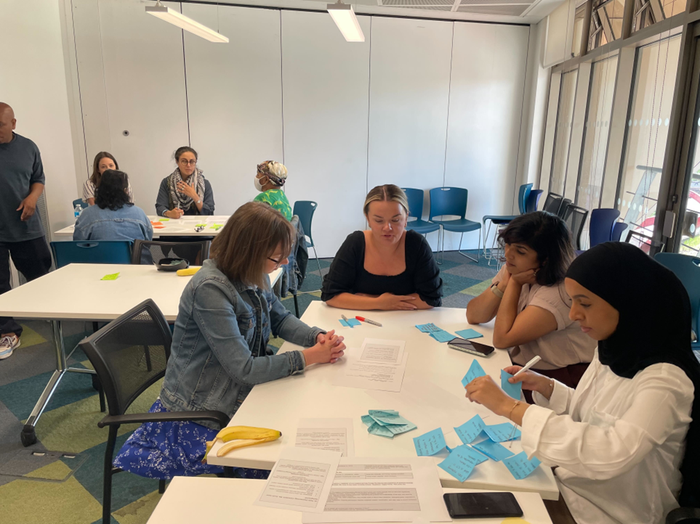
In response, Blood Cancer UK partnered with The Social Innovation Partnership (TSIP) to take a different approach: one grounded in community, trust, and lived experience. At the heart of this project were four Community Researchers — Rehab, Ngozi, Sabahat, and Yewande — each of whom brought personal experience of cancer and strong connections within their communities.
People living with blood cancer offer more than data; they share stories, trust, and the hope that their lived experience will advance research and lead to real-world solutions
- Yewande
Together, they helped shape every stage of the project: listening to the experiences of people affected by blood cancer and of health care professionals, surfacing barriers to trial participation, co-designing solutions, and holding the process accountable to those most affected by its outcomes. What follows are reflections from each of them — offering a window into the work, the challenges, and what they believe must come next.
We asked Rehab why lived experience matters in research.
She told us that clinical trials don’t exist in a vacuum — they impact real people, and for too long, those people haven’t been included in designing how trials are accessed or explained. Our project took a bottom-up approach. We started by listening — really listening — to people’s stories, challenges, and insights. From community outreach to mapping out the problem and exploring potential solutions, each step was shaped by lived experience. It wasn’t perfect, but through this lived experience-led process, we uncovered insights that traditional research methods alone would likely have missed. We learned about deep-rooted mistrust in clinical trials stemming from historical exclusion, culturally specific misconceptions about research, and real-world access barriers like language, faith-based considerations, and logistical challenges (e.g. trial timings or location).
Ngozi reflected on the challenges we faced in engaging different communities.
“We saw more interest from the Black community, but engagement from the Pakistani community took longer. We had to shift how we worked — going into community spaces, showing up without an agenda, just to listen. When it came to understanding how people wanted to receive information, it was apparent that a one size fits all approach would not be effective. People expressed a preference for different communication formats. For some, it was group conversations; others wanted one-to-one time or digital materials to explore in their own space. There was no one-size-fits-all. But when we listened, and when we were flexible, people opened up.”
“A lot of traditional outreach just doesn’t land, especially when people don’t see themselves in the system. So we flipped it. So instead of asking people to come to us, we went to them. We consulted trusted local organisations to try to understand more about barriers to engagement. We also changed how we talked — simplifying medical language, finding and cutting out jargon, holding one to one calls with potential participants in Urdu, and focusing more on listening than explaining. While we used social media to build awareness, we knew that in-person relationships would carry the trust needed for meaningful engagement. That mix of cultural sensitivity, adaptability, and accessibility was essential to creating spaces where people felt like they belonged”.
And for Yewande, the very important question was what happens next.
“The statistics highlighted by Blood Cancer UK show that Black and Pakistani people living with cancer remain significantly underrepresented in clinical trials, not just historically but right now. This is a contemporary crisis. Listening to participants made it clear: the barriers are not only systemic but deeply emotional. Participation carries hope that something might change, that someone is finally paying attention.
"In these moments, an emotional contract is formed. People living with blood cancer offer more than data; they share stories, trust, and the hope that their lived experience will advance research and lead to real-world solutions that make a difference to others like them.
What comes next must speak with the same care we asked of others. Real change is not measured in reports, but in relationships that continue, in trust that is renewed, and in communities that feel seen long after the project ends.”
Find out more about this project and get involved
We aim to improve awareness and access to blood cancer clinical trials for minority ethnic groups. To help us to achieve this goal we need support from healthcare professionals, academics and researchers.
