Harnessing the power of T-cells in stem cell transplants
The Midlands
We chatted to blood cancer researcher, Dr Sarah Dimeloe about her latest myeloma project, which has looked at harnessing the power of T-cells in stem cell transplants.
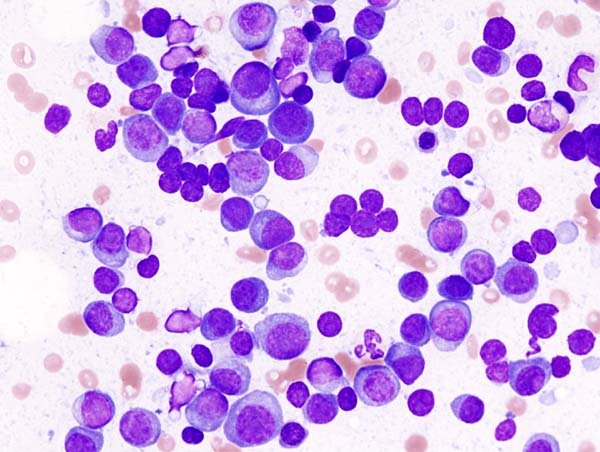
Myeloma cells
Stem cell transplants can be a life-saving treatment for people with myeloma, a type of blood cancer that can be treated but currently has no cure.
These transplants replenish the immune system with new healthy immune cells from a donor. These cells then divide and multiply replacing the patients damaged blood and immune cells.
Unfortunately, sometimes the immune cells don’t multiply enough to be able to seek out and destroy all the cancer cells, and patients can also remain vulnerable to infections.
Alternatively, the opposite can happen where the immune cells grow and multiply too much, becoming overactive, and can begin attacking the bodies’ own tissue.
The role Dr Dimeloe’s research plays
Dr Sarah Dimeloe and her team at the University of Birmingham are researching this. They’re looking to understand what causes immune cells to divide and multiply after a stem cell transplant.
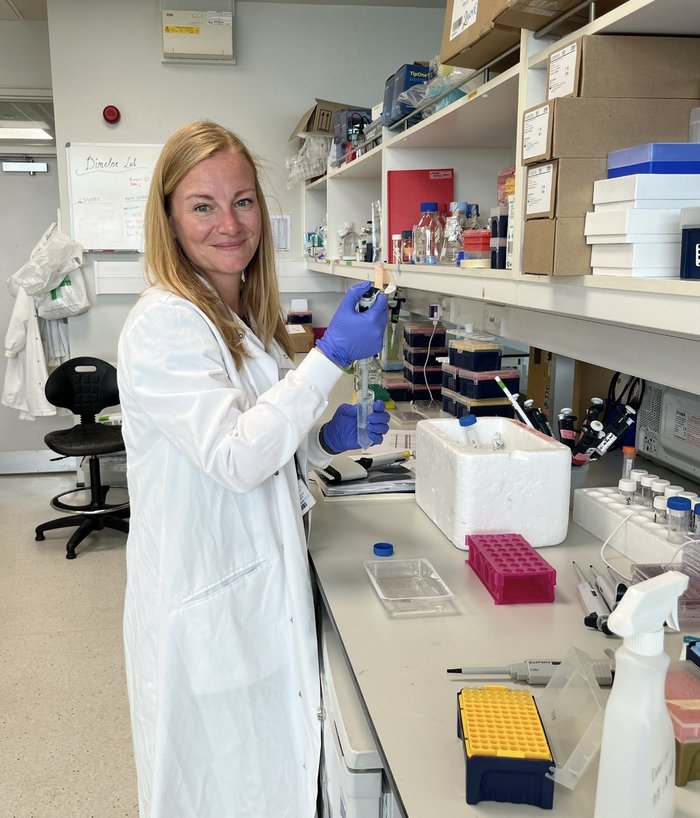
Dr Sarah Dimeloe
"In the lab we found T-cells, which are a part of our immune system, absorb a lot of nutrients to help them grow. We think some of the key processes inside the cells that control this growth could be influenced by existing drugs. One of these drugs is rapamycin, which might be able to help slow down and stop the immune cells from growing and multiplying too quickly.” - Dr Sarah Dimeloe
To confirm these findings, the team also analysed real patient data from previous research studies. Here they found this same process happening in patients who had received a stem cell transplant.
“Understanding how immune cells grow following a stem cell transplant is crucial to ensure the T-cells divide and multiply enough to seek out and destroy all the cancer cells, but not so much that they begin attacking the patient’s own tissues.” - Dr Sarah Dimeloe
The key process Dr Dimeloe and her team have identified could help to develop better treatments, improving outcomes for patients who receive a stem cell transplant.
Future treatments might even allow doctors to be able to fine-tune this process, either slowing down or speeding up T-cell growth when necessary.
But Dr Dimeloe and her team won’t stop here. They are working together with other leading blood cancer researchers to understand whether these processes are similar in other immune cells.
“The future for immunotherapy is bright. We’re excited to continue to increase our understanding of how we can use the body's immune system in the treatment of blood cancers, pushing the boundaries of what is possible to improve treatment options for patients with all types of blood cancer.” - Dr Sarah Dimeloe.
Dr Dimeloe’s ambitions are to see how this research will benefit patients with all types of blood cancers who undergo a stem cell transplant, whether that’s leukaemia, lymphoma, not just myeloma. By improving our understanding of how the immune cells regenerate following a stem cell transplant, there is the opportunity to make this treatment more effective, reduce side effects and improve patients’ recovery.

