T-cell prolymphocytic leukaemia (T-PLL)
T-cell prolymphocytic leukaemia (T-PLL) is a type of blood cancer that affects white blood cells (lymphocytes) and stops your body producing other blood cells.
What is T-cell prolymphocytic leukaemia?
White blood cells called lymphocytes are an important part of our immune system, protecting us from infection.
Prolymphocytes are lymphocytes at an earlier stage of development. They are large, immature cells that are not ready to fight infections properly. It’s these cells that are affected by prolymphocytic leukaemia.
T-cell prolymphocytic leukaemia (T-PLL) is a very rare type of blood cancer. It affects around 70 people in the UK each year.
In T-PLL, abnormal prolymphocytes grow out of control and stop your body producing other types of blood cell such as red blood cells, which carry oxygen around the body, and platelets, which help your blood to clot.
Symptoms of T-PLL
Some people have no symptoms when they are first diagnosed with T-PLL. Others may have one or more of these symptoms:
- shortness of breath, chest pain or cough, caused by fluid around the lungs
- fluid collecting in your legs or stomach area, so you feel heavy or bloated
- breathlessness and paleness (pallor), caused by low red blood cells
- bruising and unusual bleeding, caused by low platelets
- stomach pain, feeling uncomfortably full or feeling sick, because your spleen or liver is swollen
- swollen lymph nodes (glands), most easily felt in your neck, armpits or groin
- skin rashes
- swelling around the eyes.
See our information about blood cancer symptoms for more information, including how symptoms can look different depending on your skin tone.
You may also have one or more of these symptoms, called B symptoms:
- extreme tiredness (fatigue)
- losing weight without trying
- night sweats that soak your clothes and bedding.
Tests for T-PLL
Your doctor will examine you to check if your lymph nodes, liver and spleen are swollen, and look at any rashes on your skin. You will also have a range of blood tests:
- to count how many of each type of blood cell are in your blood (full blood count)
- to look for abnormal T-cells
- to look for specific genetic changes in your T-cells
You are likely have an X-ray or CT scan to look at your chest, stomach area or pelvis (the ring of bones that connects your hips to your spine.)
You may also have a lymph node, bone marrow or skin biopsy. Biopsies are where a doctor takes a small sample of tissue to look at under a microscope.
We have more information about blood cancer tests including biopsies and scans.
Active monitoring
If you have no symptoms when you are diagnosed with T-PLL, or the symptoms are mild, you may not need treatment right away. Instead, your doctor may recommend that you have active monitoring – regular check-ups to see whether the T-PLL is staying the same or developing.
It can feel strange to be told you don’t need treatment yet. It might help to connect with other people who are on active monitoring on our online community forum.
Get a weekly support email from us
We'll send you clear and simple information, practical tips, and advice from other people with blood cancer, to help during the first few weeks and months after diagnosis.
Treatment for T-PLL
Currently, treatment for T-PLL is unlikely to cure it. Rather, it aims to put you into remission, where this is no sign of the cancer, or it stays at a low level with few symptoms.
Alemtuzumab
The standard treatment for T-PLL is a targeted drug called alemtuzumab. Alemtuzumab is a type of drug called a monoclonal antibody. It attaches to a particular protein on the surface of T cells and kills them.
Alemtuzumab is given through a drip into your vein (intravenous infusion).
Stem cell transplant
If you go into remission after alemtuzumab, you may be offered a stem cell transplant. This might use stem cells from a matched donor (a donor or allogeneic transplant). Or it might use healthy stem cells collected from your own body (an auto or autologous transplant).
A stem cell transplant means having high-dose chemotherapy to kill any remaining lymphoma cells before the collected stem cells are introduced.
You will need to be generally quite fit to have a stem cell transplant. It is a very intensive (strong) treatment and isn’t suitable for everyone. Your doctor will talk to you about whether a stem cell transplant is an option for you, and explain the risks and benefits.
Your infection risk
T-PLL affects white blood cells that normally help you fight off infections. So you are likely to be at higher risk of getting infections that last longer and are more serious than usual.
Treatment also stops your body fighting infections effectively.
Even if you are on active monitoring, you are likely to be at risk from infections.
Your hospital team may give you medicine to protect you, such as antibiotics to stop you getting bacterial infections. You may have an antiviral medicine called aciclovir to prevent shingles.
There are also things you can do to help yourself. Read our information about how to protect yourself against infections and order some free infection alert cards so you and your family know what to do if you get symptoms of an infection.
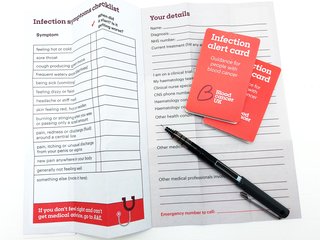
Order your free infection alert cards
With our pocket guide you can record infection symptoms and personal details to share with medical staff. Find out what to do and what to say if you go to A&E.
If the T-PLL relapses
If the T-PLL comes back after your first round of treatment, you may be offered alemtuzumab again, if it worked well the first time. Or you may have alemtuzumab along with a chemotherapy drug such as pentostatin.
If this treatment doesn’t work, your doctor may see if there are any clinical trials you can join. A clinical trial gives you the chance of having a new treatment that may be better than standard treatments.
Because T-PLL is so rare, there aren’t many trials available in the UK. Doctors are trying to change this. But if there are no more treatment options for you, you may be offered palliative care.
Palliative care aims to manage your symptoms and keep you comfortable, but will not treat the T-PLL directly. Palliative care teams can also refer you to support services to help you manage the physical and emotional effects of T-PLL and its treatment.
Treatment side effects
Treatment for T-PLL can cause a range of different side effects, but you won’t have all of them. The side effects will depend on which drugs you are taking and how you personally react to them.
Everyone is different – even two people on the same treatment can have a different experience.
We have more information about some common side effects of blood cancer treatment:
- sore mouth or gut (mucositis)
- fatigue
- sickness and vomiting
- brain fog
- hair loss
- nerve damage (neuropathy)
- eating problems
- fertility problems
Tell your hospital team as soon as you notice a change in how you feel. They will give you self-help strategies and may offer you medicine to ease the effects of treatment, such as anti-sickness medication.
Side effects can affect your emotional health too. Talk to your hospital team about how you are feeling mentally. Or read our information about mind and emotions to find out where you can get help.
Prognosis for T-PLL
T-PLL is usually a fast growing blood cancer. At the moment, there are only a few treatments for T-PLL, so there are limited options if your first treatment doesn’t work.
If you would like to know about your prognosis (what is likely to happen in the future), your hospital team are the best people to ask. They know your test results and your personal situation. Think about what questions you might want to ask them.
If you would like support to have a conversation about your prognosis, our Support Service nurses can help.
Living with T-PLL
A blood cancer diagnosis can affect your life in many ways: your mental health, your financial situation, your plans for the future. It will also affect the people you love.
You may find it helpful to read our information on these topics:
- mind and emotions, including self-help tips and accessing counselling
- money, work and other practical advice
- guidance on eating well with blood cancer
- the benefits of keeping active
- information for family and friends.
Call our Support Line nurses free on 0808 2080 888 or email [email protected] to talk through any concerns or ask questions.

Join our Online Community Forum
Use our supportive Online Community Forum to connect with others affected by blood cancer and share your experiences. You can also explore our 'ask the nurses' threads to hear from our nurses about topics such as active monitoring.
More About ThisAbout this information
First published January 2026. Next full review due January 2029. We may make factual updates between reviews.
We would like to thank Consultant Haematologist Dr Dima El-Sharkawi for checking the clinical accuracy of this information.
