Treatment for T-cell lymphoma
T-cell lymphoma is usually treated with chemotherapy, and you may be offered the chance to join a clinical trial.
Clinical trials
Doctors often recommend that people with T-cell lymphoma should be treated as part of a clinical trial.
Clinical trials are research projects involving patients. New treatments for blood cancer are being developed all the time, and clinical trials are designed to test them in a safe and careful way.
If you are treated through a clinical trial, you will be offered either the best current treatment, or one that may be even better. Read more about clinical trials.
Treatment types
Treatments for T-cell lymphoma vary depending on the specific disease type. Your hospital team will talk through the treatment options based on your personal circumstances.
CHOP chemotherapy
Treatment is often chemotherapy based on a combination of drugs called CHOP:
- C - cyclophosphamide
- H - doxorubicin (also called hydroxydaunorubicin)
- O - vincristine (formerly called Oncovin)
- P – prednisolone (a steroid)
You may have a slightly different combination of drugs, but CHOP is the basis of most combinations. It is given through a drip into a vein (intravenous infusion), apart from prednisolone, which is taken as a tablet.
Stem cell transplant
A stem cell transplant may be an option for some people with T-cell lymphoma. This will use either your own healthy stem cells (auto or autologous transplant), or cells from a matched donor (donor or allogeneic transplant).
A stem cell transplant involves high-dose chemotherapy to kill any remaining lymphoma cells before the healthy stem cells are introduced. It is a very intensive (strong) treatment and isn’t suitable for everyone.
Your doctor will talk through whether a transplant is a good option for you.
Treatments by type of T-cell lymphoma
Ask your hospital team about the treatment they are recommending and why it’s best for you.
Find your diagnosis below for more information about specific treatments, or contact our Support Service on 0808 2080 888 or [email protected]
Treatment depends on the type of ATLL you have.
- You may be treated with AZT and interferon. AZT is an antiretroviral, a drug used to control diseases caused by viruses. Interferon is a manufactured version of a type of protein made in our bodies. AZT is taken as a tablet or capsule. Interferon is injected under the skin.
- You may have CHOP chemotherapy. Some people have AZT and interferon alongside CHOP.
- People who are fit enough may be offered a donor stem cell transplant.
If you have ATLL but don’t have any symptoms, you may not need treatment straight away. You will stay under the care of the hospital and have regular check-ups until things change. This approach is called active monitoring.
The treatment for AITL is the same as for peripheral T-cell lymphoma (NOS).
- Most people will have CHOP chemotherapy.
- Some people may have radiotherapy to affected areas of the body, if the lymphoma is early stage.
- If you are fit enough, you may be offered an auto stem cell transplant.
- If there is a risk of the lymphoma spreading to your brain or spinal cord, you may have treatment to stop this happening. This is usually with a chemotherapy drug called methotrexate which is injected into the spine.
- ALCL is usually treated with CHP chemotherapy (cyclophosphamide, doxorubicin and prednisolone) along with a targeted drug called brentuximab vedotin (BV). These drugs are given through a drip into a vein (intravenous infusion) except for prednisolone, which is a tablet.
- BV works by attaching itself to lymphoma cells and releasing a chemotherapy drug directly into the cell. This is a type of treatment called an ADC (antibody drug conjugate).
- You may be offered an auto stem cell transplant, depending on your overall level of fitness.
- You may have radiotherapy to affected areas of the body, if the ALCL is at an early stage.
- You are likely to have a combination of chemotherapy drugs including either L-asparaginase or cisplatin. These work better than other drug combinations for this type of lymphoma.
- Some chemotherapy combinations include a drug called methotrexate. This helps to stop the lymphoma spreading to the brain and spinal cord.
- If you have early stage disease, you may also have radiotherapy to specific areas of your body.
- You may be offered either an autologous or donor stem cell transplant if the lymphoma is late stage, and if you are fit enough.
- Most people will be treated with CHOP chemotherapy.
- Some people will have treatment with the Newcastle regimen. This involves two types of chemotherapy – CHOP followed by IVE (ifosfamide, etoposide and epirubicin), and then an autologous stem cell transplant.
The treatment for PTCL-NOS is the same as for angioimmunoblastic T-cell lymphoma (AITL). Treatments for follicular T-cell lymphoma and nodal peripheral lymphoma with TFH are also the same.
- Most people will have CHOP chemotherapy.
- Some people may have radiotherapy to affected areas of the body, if the lymphoma is at an early stage.
- If you go into remission (where there is no sign of the lymphoma left) you may have an autologous stem cell transplant.
- Rarely, there may be a risk of lymphoma spreading to the brain or spinal cord. A drug called methotrexate can stop this happening, but most people won’t need this treatment.
Your infection risk
T-cell lymphoma affects white blood cells that normally help you fight off infections. So it’s very important to understand that you may be at higher risk of getting infections that last longer and are more serious than usual. Treatment also stops your body fighting infections effectively.
Your hospital team may give you medicine to help with this, including:
- antibiotics to stop you getting bacterial infections
- injections of a drug called GCSF (granulocyte colony stimulating factor) to help you produce more white blood cells
- an antiviral medicine called aciclovir to prevent shingles.
There are things you can do to help yourself. Read our information about how to protect yourself against infections and order some free infection alert cards so you and your family know what to do if you get an infection.
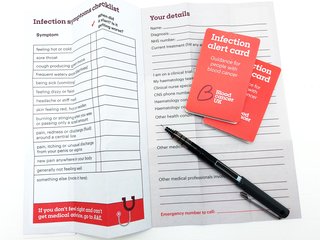
Order your free infection alert cards
With our pocket guide you can record infection symptoms and personal details to share with medical staff. Find out what to do and what to say if you go to A&E.
Treatment for relapsed T-cell lymphoma
If the lymphoma comes back after your first treatment (relapses), you will be offered more treatment. This could be the same treatment again, if it worked well previously. If the lymphoma didn’t respond to the first treatment or it relapsed quite quickly, you may be offered a different treatment. Often this will be a different combination of chemotherapy drugs.
Another option is palliative care. This is not the same as end-of-life care. While it won’t cure the lymphoma, palliative care aims to manage your symptoms, reduce pain, help you live longer and generally improve your quality of life.
Your hospital team will talk through your options for further treatment if you have a relapse.
Treatment side effects
Blood cancer treatment can cause a range of side effects. The side effects of your treatment for T-cell lymphoma will depend on which drugs you are taking. But everyone is different – even two people on the same treatment can have a different experience.
We have more information about these common side effects of blood cancer treatment:
- sore mouth or gut (mucositis)
- fatigue
- sickness and vomiting
- brain fog
- hair loss
- nerve damage (neuropathy)
- eating problems
- fertility problems
If you are having treatment, tell your hospital team as soon as you notice a change in how you feel. They will recommend medicines and self-help strategies to help with side effects.
Side effects can affect your mental wellbeing as well as your physical health. Talk to your hospital team if you are feeling low. Or contact our Support Service to find out how to get help.
Our research
Our £500 million investment in research since 1960 has helped transform treatments and taken us to the point where beating blood cancer is now in sight. Our researchers are working to finish the job.
More About This