What to expect on a clinical trial
If you’re considering joining a clinical trial but are still unsure what it all means, learn what happens before, during and after enrolling. This page also contains more information about how your safety and wellbeing is prioritised.
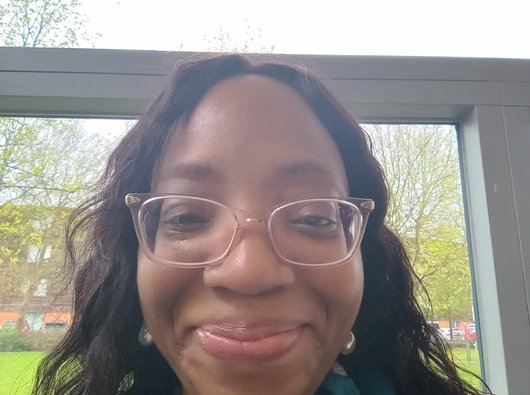
Watch Precious talk about her experience on a clinical trial, and hear what she’d choose to tell other people from Black, Pakistani and minoritized communities about clinical trials.
Watch Precious talk about her experience on a clinical trial, and hear what she’d choose to tell other people from Black, Pakistani and minoritized communities. This video contains Urdu subtitles.
Finding a trial
Your doctor may raise the possibility of taking part in a clinical trial if they know about one that might be suitable for you. However, if they don’t mention it, it doesn’t mean that you can’t join a trial or that there isn’t one available. Lots of people tell us that they had to ask about trials, or search online and find something themselves.
Finding a trial yourself can be difficult, and sometimes the information available to the public is hard to understand. Our Clinical Trials Support Service can help you search for a trial and see if any of the results could be an option for you.
If you do wish to look at online trial databases, we recommend:
- Be Part of Research
- Home | ClinicalTrials.gov
- Find a clinical trial | Cancer Research UK
- Clinical Trial Finder | Find trials related to the treatment of myeloma (if you have myeloma)
- Lymphoma Action | Find a trial (if you have lymphoma)
You should be able to find information in these databases about where trials are being carried out, whether a trial is open to recruiting new people, who can take part in a trial, and who to contact with any questions about a trial.
If you see a clinical trial on a database that you’re interested in joining or hearing more about, you’ll need to discuss it with your doctor or cancer specialist. Usually, having a referral from your doctor is the only way you can enrol on a trial.
We know that the thought of going on a clinical trial can be confusing and sometimes scary for some people, but support is available if you or your loved ones have any questions or concerns. If you don’t feel comfortable speaking to your doctor, you may like to give our Clinical Trials Support Service a call first. Our nurses can explain more about clinical trials and what to expect, and help you plan what to say when you’re ready.
We also have more information about what a clinical trial is and what the benefits and risks are.
"It can be hard to find out about trials unless someone else brings it up. It’s important this changes, so more people from Black and other ethnic communities get to have the experience that I did. Don’t be afraid to ask if there is a trial for you."
Precious, diagnosed with chronic myeloid leukaemia (CML). Read more stories from people affected by blood cancer.
Eligibility and recruitment
All trials have guidelines about who can and can’t take part. These guidelines are called eligibility criteria, and can include characteristics such as your diagnosis, treatment history and general health.
Eligibility criteria are used to make sure that the trial:
- includes people who may benefit from the treatment
- keeps everyone involved in the trial safe
- doesn't result in anyone taking an avoidable health risk.
It’s important for your own safety and the success of the trial that you meet all the trial criteria. By only including people who meet the criteria, the trial also avoids getting results that could confuse or invalidate its overall findings.
Most eligibility criteria will be explained to you before you enrol on a clinical trial. However, it may not be possible to know for sure if you are a suitable candidate at this stage. Many trials include pre-trial tests or screenings to confirm your eligibility, which can only be carried out once you’ve agreed to enter the trial.
It’s normal to feel upset and disappointed if you don’t meet the eligibility criteria of a trial, especially if you enrol and go through any pre-trial tests. However, if this happens, your doctor or the trial research team will tell you about any alternative options available to you. They may even be able to recommend a different trial.
Time commitment
If you are accepted onto a clinical trial, you’ll be monitored regularly during the trial and maybe after it ends as well. This could mean you’ll need to go to hospital or a clinic more often than you would normally. It’s worth asking your doctor, CNS or the trials team how regularly you’ll need to attend appointments, so you can consider how convenient this will be for you.
You might need to think about:
- how you’ll travel to the hospital, and how much this will cost
- whether you’ll need any extra support, for example with childcare
- your mental and physical health, and how you’ll manage any symptoms or side effects
- changing how you usually work or study.
We have more information about help with costs and working with blood cancer. Some clinical trials will offer to pay for any travel expenses – have a look at your patient information sheet, or ask the trials team if it’s unclear.
“I’m in a WhatsApp group for people with blood cancer that I found online. I like to go there to find things out and hear other people’s experiences. It helps me feel more informed, which means it’s easier to make decisions with my doctor."
Farman, diagnosed with myeloma. Read more stories from people affected by blood cancer.

Tests
If you take part in a clinical trial, you’ll be tested regularly to monitor the treatment and how well it’s working.
Most people on a clinical trial will need to have regular blood tests. Some people may also need extra tests (like bone marrow testing) or scans (like CT or MRI scans). This depends on the type of blood cancer you have and the treatment offered on the trial.
It’s likely that you’ll need to have your tests or scans at the trial site, but it may be possible to have some or all of them at your usual hospital. Check with the trial researchers if you’re unsure. Some trials will have funding to help with the cost of travel and any overnight stays that are necessary whilst having tests. We also have more information about help with costs, if this is something you’re worried about.
Lots of people say that having regular tests or scans during a trial is reassuring, as it provides peace of mind.
However, it’s worth thinking about the time commitment involved, and if you think you’ll need any additional support. Don’t be afraid to ask your doctor or the trial team what tests you’ll need, how often you’ll need them, and where you’ll need to go. They should also be able to tell you how you’ll get your results, and what to expect from them.
Your prognosis
Everyone is different and responds to treatment differently. This is true whether the treatment you are receiving is part of a clinical trial or not. Although the researchers in charge of a trial hope that a drug or treatment will behave in a certain way, they cannot guarantee it will work exactly the same for everybody. This is partially what a clinical trial is testing.
Your prognosis is personal to you, and your doctor will be able to tell you more about what you can expect. Generally speaking, how you respond to a drug or treatment depends on lots of things, including:
- your age
- your general health
- the type of blood cancer you have
- how advanced the blood cancer is
- any treatment you’ve had before
- genetic markers or mutations specific to you, which can influence how a treatment works.
If you find that a new drug or treatment doesn’t work for you, it can be hard to understand and accept. Let your doctor, CNS or the trial researchers know about any worries or concerns that you have. They will be able to support you at every stage of the trial, including leaving a trial if things don’t work out as hoped. You can also speak to us, or join our community forum to connect with people in a similar situation.
Leaving a clinical trial
Being on a clinical trial is a positive experience for most people, but if you change your mind after being accepted or don’t want to stay on a trial after enrolling, you can leave at any time.
Your doctor will explain what leaving a trial could mean for you, your treatment and your prognosis, so you can make an informed decision. Usually, you’ll have to stop taking the treatment offered on the trial if you leave, but you may be able to swap to an alternative standard treatment if there is one that is safe and suitable for you.
If you leave or say no to a trial, your doctor shouldn’t judge you or treat you any differently to anyone else.
About our health information
This information about clinical trials is accredited with the PIF TICK, the UK's only quality mark for trusted health information.
Last full review December 2025. Next full review due December 2028. We may make factual updates to the information between reviews.
We would like to thank Consultant Haematologist Dr Priya Sriskandarajah for checking the clinical accuracy of this information. Thank you also to everyone who participated in the community research for this project, and shared their experience of clinical trials.

Contact our Clinical Trials Support Service
Get personalised support to understand which clinical trials are available - whether you're a patient, carer or healthcare professional.
