Forget about 'robot uprisings', AI is a force for good
Professor Daniel Royston is a haematopathologist at Oxford University Hospitals NHS Trust who is using AI to help improve the diagnosis and treatment of blood cancer. Here he writes about the benefits of AI in his research.

AI imagines what a Blood Cancer UK researcher using AI in their work might look like. This image was AI generated for illustrative purposes.
AI is ever present in our world today
The majority of us use AI regardless of whether we realise it, and whether we like it or not. From social media platforms such as Instagram and Facebook, to Google Maps, to computer tools such as Spell Check and virtual assistants like Siri and Alexa. AI has been around for decades, but the rate of development and growth of AI is now surprising us all.
There is a lot of speculation and uncertainty around the use and impact of artificial intelligence or AI. I want to illustrate that when used responsibly, AI is truly a force for good in the healthcare space. But of course, I would say that... because I’m currently harnessing AI to help beat blood cancer.
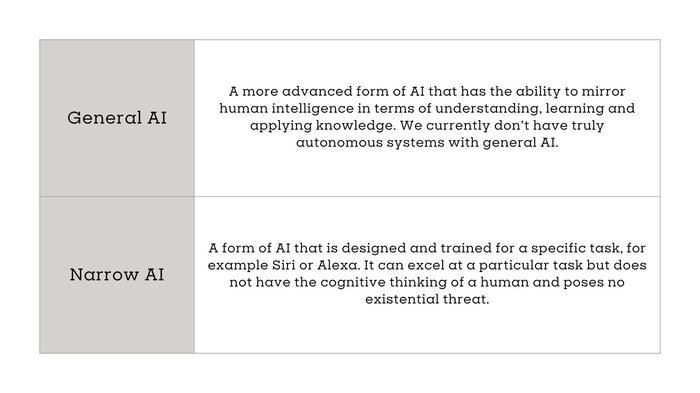
What is AI?
AI is a field of computer science that focuses on the development of computer systems that mimic a human mind’s ability to perform tasks such as learning, reasoning and problem solving.
There are 2 main types of AI:
Using AI technology in blood cancer research
My current research uses narrow AI technology to look for new ways to diagnose myeloproliferative neoplasms (MPNs), a form of blood cancer, making it quicker and easier to reach an accurate diagnosis and help predict how it will behave in individual patients.
Before we go any further, I should probably make it clear -- I'm not an AI expert... I’m a doctor who applies narrow AI in my research.
My hope is that within the next 10 years, we will begin to see the widespread use of AI to help and improve the diagnosis of many diseases. I believe AI will become more and more important as a tool to handle large amounts of data from individual patients and patient groups in the future, speeding up diagnosis, treatment and the search for new therapies.
How I’ve harnessed AI to treat MPN
People with MPN are usually diagnosed after several tests including taking a bone marrow biopsy where blood cells in the spongy parts of their bone are taken away and reviewed by a specialist doctor like myself using a microscope. This takes many years of training and experience to begin to learn the specific features to look out for in making a diagnosis.
Analysing a bone marrow biopsy can be challenging even as an experienced doctor. This is because someone who has MPN may only have very subtle changes in their bone marrow biopsy compared to someone without the disease. A diagnosis of MPN sometimes depends on a doctor’s best judgement of a biopsy. But even with extensive training and practice there can be disagreements between doctors on whether to make a diagnosis. In such cases we relying on the human eye, human judgement, opening the door to human disagreements and the potential for error.
So there’s a need to develop new techniques that can allow us to more accurately diagnose the disease.
“AI is a tool that can help improve what we do as healthcare professionals, helping doctors like me to do our job better.”
It means we can use powerful computers to identify features of a bone marrow biopsy that are objective and measurable, allowing us to interpret it with more precision and give a more accurate diagnosis.
AI imagines what myeloproliferative neoplasms might look like under a microscope. This image was AI generated for illustrative purposes.
Humans are often good at making simplified decisions based on combining or merging different sets of evidence, but diagnosing MPN can involve accurately combining large numbers of little pieces of data like variations in cell appearance or subtle differences across a biopsy. The human brain is less good at handling and accurately summarising this kind of information and can be prone to errors. AI is ideally suited to help with these tasks, many of which can be fully automated.
Man and machine = the perfect team
In using AI techniques, we’re not looking to replace the doctor and the doctor-patient interaction.
There still have to be doctors like me responsible for the results of AI-based tools, to make sense of and confirm any outcome. AI has potential to support us, to allow us to work more effectively.
If there is any uncertainty about a biopsy, AI techniques can offer an independent and unbiased view. Ultimately, AI gives doctors like me more confidence that our interpretation of the biopsy is correct so we can diagnose MPNs more accurately and efficiently.
AI’s ability to notice smaller and more subtle changes will provide reassurance to doctors and patients that they have received an accurate diagnosis. More importantly, it will ensure patients are diagnosed quicker and earlier, and therefore can be treated sooner with the most effective therapies. Earlier diagnosis and treatment will give people with MPN the best chance of survival.
AI techniques will also allow doctors to more effectively determine changes in the disease over time, accurately determining if a drug treatment is working, allowing them to change the course of treatment if needed. It can also help the search for new and more effective therapies.
AI can help our NHS
The NHS is under immense stress and pressure, especially in the diagnosis of cancers. AI is already starting to be used within the NHS and has seen major developments in areas such as interpreting CT and X-ray images in radiology where it is improving the detection and diagnosis of cancers.

AI imagines doctors working together with artificial intelligence. This image was AI generated for illustrative purposes.
AI is here to stay. Rather than fear it we need to understand and embrace it and the enormous potential it has in the healthcare space. AI can be a force for good. All of us have fears and anxieties about its uncontrolled growth and expansion, but I remain confident and optimistic about its use within healthcare. However, we must be vigilant about the potential for misuse of AI technologies. As doctors and researchers, we have to play our role in making sure that what we do is responsible, fully accountable, ethical and benefits everybody in society.
AI will benefit the blood cancer community
The diagnosis of blood cancer is a very specialised area, and in the UK we don’t have enough doctors with specialist experience in the understanding of bone marrow biopsies.
AI offers a way of allowing doctors in training and those with less experience to get much needed support in the interpretation of bone marrow biopsies. Ultimately, experienced doctors will still make the diagnosis and treatment decisions, but it will ease the burden and allow us to deliver more work in our time. This makes AI extremely advantageous for the NHS economically and helps to fill gaps in service provision.
As these AI techniques don’t require people to be physically tied to particular hospitals, images of patients’ biopsies could be uploaded to a centralised system. In principle, this means everybody within the NHS who has a bone marrow biopsy could benefit from these AI techniques, regardless of where they are being treated in the UK. This will help bring equity to all patients, not just those who happen to be linked to expert centres.
Thank you for your support
My colleagues and I are incredibly grateful to the patients and their families who support our work. Without them and without our funders, including Blood Cancer UK, this research wouldn’t be possible.
Thank you,
Professor Daniel Royston