Because research can beat blood cancer in a generation
Together we’ve achieved a lot in the last 60 years. We've invested over £500million in research and improved diagnosis and treatments for people with blood cancer. But can we beat blood cancer in the next generation? Yes, and here's how...

Stopping blood cancer in its tracks
If we can, we want to be able to stop people developing blood cancer in the first place. Whilst this might not be possible for all blood cancers, it’s a very real possibility for some.
Our researchers discovered that childhood acute lymphoblastic leukaemia (ALL) can be triggered by an abnormal response to infection. We now hope it might be possible to design a preventative vaccine which could mean that some, if not all, forms of childhood ALL could one day become preventable diseases.
This is a sentiment shared by Professor Chris Bunce from the University of Birmingham. When we asked him what he thought blood cancer would look like in 30 years, he said:
“We may prevent diseases like myeloma arising in the first place.”

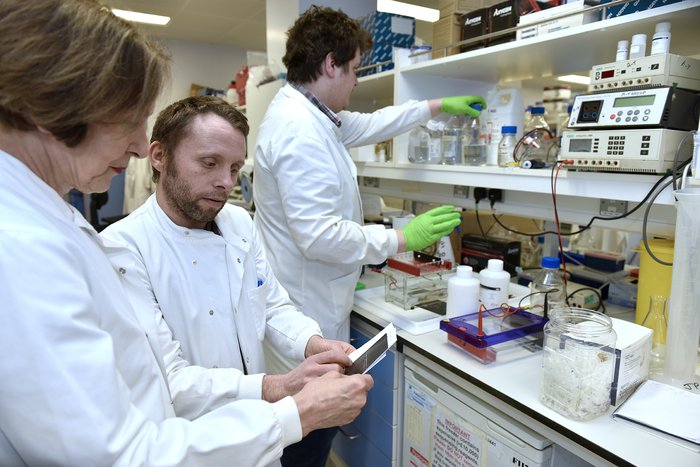
Professor Chris Bunce [left]
Chemotherapy? We want to make it history
Chemotherapy remains an important treatment for many types of blood cancer.
However, the treatment is toxic and can cause severe short and long-term side-effects. It’s not appropriate for some people with blood cancer, limiting their treatment options. In 30 years, we want chemotherapy to be a treatment of the past. This is a view shared by Dr Bela Wrench from Queen Mary University London:
“That change has already been achieved for some leukaemias such as acute promyelocytic leukaemia (APML) and I think there is promising data to indicate that this could be extended to other leukaemia subtypes. That would be a real change because it would mean fewer side effects, less time spent in hospital and therefore hopefully a better quality of life.”

Creating tailored treatments with fewer side effects
If chemotherapy is to become a treatment of the past, we’ll need new, less harmful treatments to take their place. Cancers all look different. They’re all constantly changing and evolving, and this is why treatment might work for one person but not another. What we want to be able to do is look for changes unique to every person’s cancer. If we can do this, we can tailor treatment based on the make-up of their cancer, giving them the best possible chance of survival. This isn’t just the case for blood cancer, but all cancers.
Professor Constanze Bonnifer from the University of Birmingham, agrees with this:
“Every type of blood cancer needs a different therapy.”
“In 30 years, we will know which therapies we will need to use for which blood cancer type. We will have a completely new tool-box available to target genes and proteins in cancerous cells that are required for the growth of abnormal cells.
“Blood can be easily studied experimentally, therefore studies of haematological cancers pave the way for applying the same strategy to all other cancers.”
This is also a sentiment shared by Professor Jacqueline Boultwood from the University of Oxford:
“Personalised medicine will be routine, and we will be able to target each person’s cancer with specific treatments designed on the cancer’s specific genetic make-up.”
Professor Bunce agrees, and also believes that these targeted treatments will come with fewer side effects:
“This will include new treatments with less toxic side effects that deliver either cure or long-term survival with few, if any symptoms. We will be better at diagnosing blood cancer sooner, allowing earlier treatments.”

Professor Constanze Bonnifer
Targeting the root cause of the disease
In 1999, Blood Cancer UK-funded scientist Professor Tessa Holyoake found the stem cell which creates a stream of cancerous cells in people which chronic myeloid leukaemia (CML). Blood cancer stem cells are special cells which can ‘self-renew’. They can make clones of themselves continuously, meaning that these cells give rise to a steady stream of more cancerous cells. To beat blood cancer, these cells are the ones we want to be targeting. If we can destroy the root cause of the disease, we should be able to stop cancer growing once and for all.
Professor Georges Lacaud from the University of Manchester believes we will be able to do this in the next 30 years:
“I believe in 30 years we will be able to eradicate most blood cancers by specifically targeting cancer stem cells. This will require a better understanding of the specific and unique mechanisms sustaining the self-renewal of different types of blood cancer stem cells.”
Professor Boultwood is currently working on exactly this. Her team hopes to identify changes in these cells that could be targeted by drugs, giving people with the disease the best chance of survival:
“In the next 30 years, we will have a complete picture of why and how blood cancers, develop and progress, and how we can target them effectively. Curative treatments may be available for many blood cancers.”
Collaboration
Beating blood cancer will be a global effort. It will require researchers from all corners of the world to share knowledge and findings if we’re going to beat all blood cancers.
Professor Bertie Göttgens from the University of Cambridge believes this will happen and will help drive forward research and treatment:
“I envisage a much more networked approach [to diagnoses and treatment], where a local hospital can rely on international expertise to provide rapid and accurate diagnoses, and to find appropriate treatment plans.”
Dr Wrench also adds: “[I also hope to see] greater diversity and equality in institutions and scientists delivering the research as well as those participating in research trials through [organisations] committing to fair opportunities for all.”
More people are surviving blood cancer, we’re getting better at diagnosing the disease and people are receiving kinder treatments with fewer side effects but there’s still so much more to be done.
Because we’re determined to beat blood cancer within a generation.
Thank you to our blood cancer research community for their contributions to this blog.