Mpox (monkeypox) and blood cancer
Mpox (previously called monkeypox) is a rare infection most commonly found in central and west Africa. Since 2022, there have been mpox cases in countries outside of these regions, and a small number in the UK.
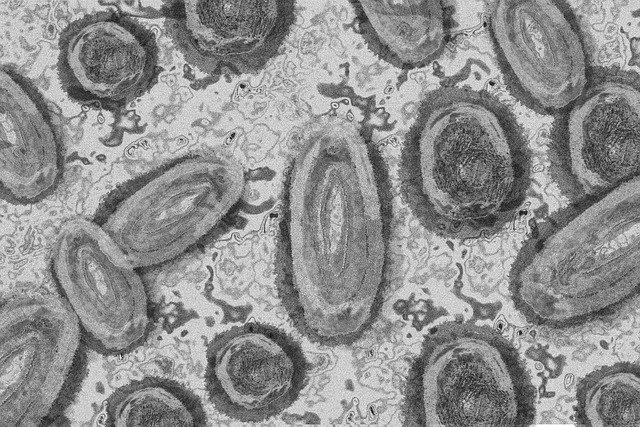
Abstract representation of the mpox virus down a microscope.
Page updated 10 September 2024
On this page
What is mpox (monkeypox)?
Mpox (monkeypox) is a virus that can affect animals and humans. It can spread from animals to humans, and it can spread from human to human.
Mpox is a virus from the same family as smallpox, which is the only infectious disease in humans to ever be totally eradicated. This was done through worldwide vaccination and surveillance.
Mpox (monkeypox) is common in central and west Africa, where animals that carry mpox commonly live. Prior to 2022, most cases of mpox were in the Democratic Republic of the Congo and Nigeria.
Since May 2022, cases of mpox have been reported in multiple countries that have not previously had mpox, in and outside of Africa.
Mpox Clade I and Clade II
Like with all viruses, there are different 'strains' of the virus. There are two main genetic groups (clades) of mpox - Clade I and Clade II.
In 2022-23, there was a global outbreak of Clade II mpox, including some cases in the UK. People who had not travelled to west or central Africa were being diagnosed with mpox in other countries. It was spread through close personal contact between people, particularly through sexual contact and other skin-to-skin contact.
Clade II mpox appears to be a less severe strain of the virus. It is still present in the UK, but is not classified as a "high consequence infectious disease (HCID)" - a measure that the UK uses to highlight diseases that have a high risk for the population and require specific prevention and control measures for suspected cases.
In 2024, Clade I cases began to be reported in new countries in Africa, outside of the five African countries it was previously only known to circulate in.
Clade I mpox tends to cause a more severe form of the disease and is classified as a "high consequence infectious disease (HCID)" in the UK. There are currently no cases of Cade I mpox in the UK.
What is the risk to people with blood cancer?
People with blood cancer may have a weakened immune system, due to the blood cancer itself or its treatment. That means that catching mpox carries more of a risk, as your body might be less able to fight off the virus. This is the same for any virus, as people with blood cancer are at higher risk from infections.
At the moment, mpox in the UK is still extremely rare. It’s important to keep things in perspective, and to continue thinking about common infections such as flu or covid, which continue to be a bigger risk to people with blood cancer.
The risk of catching mpox in the UK is low. As of August 2024, the milder Clade II mpox is still present in the UK, but there are no known cases of the more worrying Clade I mpox.
If you think you have symptoms of mpox, tell your doctor or a sexual health clinic as soon as possible. Even if you don’t have mpox, any unusual symptoms should be checked, as you might have another virus or infection.
Some practical things you can do to protect yourself include:
- Be aware of the symptoms of mpox, particularly if you are sexually active and especially if you have new sexual partners.
- Avoid travel to west, central or east Africa if possible. If you do go, avoid wild/stray animals and close contact with people you don't know, and watch out for mpox symptoms after returning home.
- Get all the vaccinations you are eligible for, including covid vaccines, flu jabs and pneumonia vaccination.
- If you are sexually active in London or Greater Manchester, or live or work in those areas, you may be eligible for an mpox vaccine
- Be aware of the risk of infection in general for people with blood cancer and take steps to reduce your risk of infection.
Mpox (monkeypox) symptoms
Mpox (monkeypox) symptoms include:
- a rash that starts as raised spots, which turn into sores (ulcers) or small blisters filled with fluid. The blisters eventually form scabs which later fall off.
- high temperature (fever)
- headache
- muscle aches
- backache
- swollen glands
- shivering (chills)
- exhaustion
- joint pain.
If you get infected with mpox, it usually takes between 5 and 21 days for the first symptoms to appear.
The mpox rash often develops on the face, palms of the hands and soles of the feet. It can also develop on the mouth, genitals and eyes.
How mpox (monkeypox) spreads
People with mpox are infectious while they have symptoms. You can catch mpox through close physical contact with someone who has symptoms. The rash and scabs are especially infectious. Clothing, bedding, towels or things like cutlery and cups can also carry the virus from one person to another. The virus can also spread through saliva.
Anyone who has close physical contact with someone who has symptoms of mpox could catch the virus. People who were vaccinated against smallpox probably have some protection against mpox infection, but they could still catch it. Smallpox vaccinations were used in the UK until 1971.
If you get symptoms of mpox (monkeypox)
If you think you have symptoms of mpox or have been in close contact with someone who might have mpox, tell your doctor, self-isolate if you can, and avoid close contact with others.
Mpox (monkeypox) treatment
Mpox (monkeypox) usually gets better on its own. There aren’t any specific treatments routinely used for mpox, but a smallpox vaccination could help reduce symptoms. Other options include antivirals such as Tecovirimat and Cidofovir. There are hospitals around the UK that specialise in treating imported illnesses such as mpox.
Mpox (monkeypox) vaccine
The NHS is currently offering the smallpox (MVA) vaccine to people who are more likely to be exposed to mpox in London or Greater Manchester. This includes:
- healthcare workers caring for patients with confirmed or suspected mpox
- men who are gay, bisexual or have sex with other men, and who have multiple sexual partners
- people who've been in close contact with someone who has mpox.
Find out more about the NHS mpox vaccination programme.
For more information about mpox, see these trustworthy sources:

Worried about anything or have questions?
If you need someone to talk to, please don't hesitate to contact our Support Service by phone or email.

