Research impact on chronic myeloid leukaemia (CML)
The survival rate for chronic myeloid leukaemia (CML) has dramatically improved over the last few decades, and we at Blood Cancer UK are proud of the role our research has played in this.
Professor John Goldman and CML
In the early 1970s scientists in the United States started showing some success with bone marrow transplants in leukaemia, and we supported Prof John Goldman from the early 1970s as he pioneered bone marrow transplantation as a treatment for chronic myeloid leukaemia (CML) in the UK.
Prof Goldman learned from what was happening in the US, where scientists had started trying to collect bone marrow cells from people with CML when their leukaemia was stable, so they could use them to treat the patient when the cancer relapsed and became more aggressive. But it proved difficult to freeze the cells for a long time without damaging them.
But then Prof Goldman made the breakthrough discovery that CML cells could be found in the blood when someone is diagnosed. This meant they could collect CML cells from blood samples, which led to being able to use a patient’s own cells in their transplant.
Investing in bone marrow transplants
Seeing the potential of bone marrow transplantation, we invested over £3 million to pioneer bone marrow transplants in the UK.
Following reports of successful transplants for CML in the US, Professor Goldman performed the first UK transplant for CML at Hammersmith Hospital in 1978, using donor bone marrow from a healthy identical twin. He then carried out the first sibling transplant for CML in 1981.
One of the challenges at this stage was graft-versus-host disease, which is a dangerous complication of stem cell transplants where the donated stem cells or bone marrow attack the body. But Prof Goldman, working with Prof Jane Apperley, took a method of removing T-cells from donor blood that was already being used for aplastic anaemia and started using it for CML. This was much safer for patients because they didn’t get graft-versus-host disease, which meant they didn’t need to take drugs that weakened their immune system.
Then in 1985, the team carried out the first transplant in patients with CML where the donor was not related to the recipient. This went well initially, but they soon realised that removing T cells to try and prevent graft-versus-host disease meant the control of the CML was not as good, and patients started to see their disease return. This meant they needed a way to detect as early as possible if patients were starting to relapse, so they could treat them quickly.
In the early 1990s, Prof Goldman was joined by Prof Nick Cross. They knew that in CML two particular genes stick together, and so by developing a way of looking for these stuck-together genes they were able to detect tiny levels of CML cells. This meant they could identify patients who were likely to relapse earlier, and which benefited the patients because they were more likely to respond to treatment the earlier they started it.
TKIs and CML
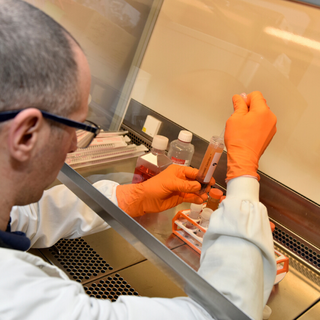
In 1996, Professor Goldman heard about a new drug called imatinib that killed CML cells. With funding from us, his team played an important role in learning how imatinib, a type of tyrosine kinase inhibitor (TKI), worked on CML cells.
At the same time, Prof Cross started to standardise methods for detecting CML so they could be used by clinics worldwide to monitor response and relapse in people with CML after they received imatinib. The technique Prof Cross developed is still used today to monitor CML patients after treatment.
The first trials of imatinib in the UK were carried out at the Hammersmith Hospital under the direction of Professor Goldman.
Prof Richard Clark had previously showed that imatinib was actively transported into CML cells via a transporter molecule on their surface. Because some people with CML did not respond to imatinib or soon stopped responding, we funded Prof Clark to study levels of the transporter molecule in CML patients. He showed that presence of the transporter molecule was clinically important, and later showed that two new TKIs called nilotinib and dasatinib did not need these transporter cells to be able to attack the CML cells. Both drugs are now approved for CML in the UK.
Professor Clark also led a Blood Cancer UK-funded trial called DESTINY, which looked at whether it was possible to reduce and then stop TKI treatment, potentially meaning patients could avoid side effects. This study showed that many people could stop taking TKIs for a number of years without their CML coming back, and those whose CML did return could return to remission by starting to take the TKIs again.
CML and stem cells
In 1999, Blood Cancer UK-funded Prof Tessa Holyoake discovered a CML stem cell. This landmark discovery gave hope that one day people with CML would be able to stop taking treatment. She followed this in 2002 by showing that there are a group of cancerous stem cells that were not killed by CML treatments, and so they could carry on producing more cancerous cells.
She was then joined by Prof David Vetrie, and in 2016 they showed that by targeting two particular genes it is possible to destroy the CML stem cells but leave normal blood stem cells unharmed. They also discovered that CML cells are sensitive to particular drugs and that when these drugs are used together with TKI drugs, the CML cells self-destruct.
CML research: the next chapter
Thanks to the work of Profs Vetrie, Holyoake, Clark, Cross, Goldman, and many others, Blood Cancer UK funding has led to new discoveries that have improved treatments for CML. These efforts, along with those of other researchers around the world, mean five-year survival for CML now stands at around 90%.
This means that many thousands more people are getting the chance to live longer, better quality lives.
But too many people are still dying of CML, and so we will keep funding research until we reach the point when everyone with CML survives. But we will only reach that day by raising the money to fund more research. Help us fund the next blood cancer research breakthrough.