Research impact on myeloma
Our research in myeloma has helped pioneer new treatments and improve existing ones
Studying chromosomes to predict outcomes
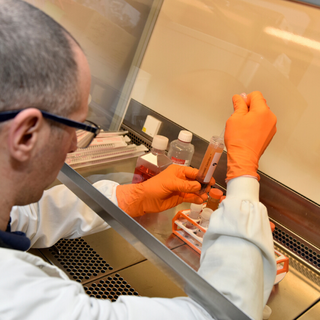
Until recently, little was known about how myeloma was likely to progress. To address this, we funded the UK Myeloma Forum Cytogenetics Group (UKMFCG) led by Dr Fiona Ross at the Wessex Regional Genetics Laboratory.
The programme was established to understand the genetic abnormalities of blood samples from people with myeloma, who had taken part in the national Myeloma IX study. The team analysed 1,140 samples from the study and linked different chromosomal abnormalities to individual patient survival. The results showed that having certain chromosomal abnormalities was directly linked to poorer survival.
Testing for chromosome abnormalities
In another study we funded, the team used its large set of samples to answer a controversial question in myeloma cytogenetics (study of chromosomes). There was disagreement worldwide about the importance of a frequently found chromosome abnormality in myeloma, whether or not myeloma cells contained chromosome 13. The team were able to show that people with myeloma, who didn’t have chromosome 13, were likely to have a poor prognosis. This confirmed that it was important for predicting the course of a person’s disease.
Based on the chromosomal abnormalities identified by the team, they went on to develop a model for predicting the prognosis of people with myeloma. As a result of Dr Ross’ research, UK clinical guidelines recommend that people with myeloma have a test for chromosome abnormalities.
Identifying inherited risk of myeloma
Research we helped to fund identified the first risk genes for myeloma. Family members of myeloma patients are known to be between two and four times more likely to develop the disease. This is in comparison to the general population.
Professor Richard Houlston at the ICR discovered the first genes responsible for some of this increased risk and estimated that they could account for more than a third of myeloma cases in European countries.
Since that first discovery, research we funded alongside Myeloma UK and Cancer Research UK has led to the identification of further twenty three genetic changes that can increase an individual’s risk of myeloma.
Understanding bone cells in myeloma
Some cancers, including myeloma, cause cancer-induced bone disease: lesions in the bone that lead to potentially catastrophic fractures. These can occur in the pelvis or thigh bone, seriously limiting the person’s mobility. We funded Professor Croucher during his time at Sheffield University, where he made important advances in understanding more about how myeloma cells become established in the bone, and how they destroy bone tissue.
In 2001, he discovered the pathway that was the driver of the bone disease that occurs in myeloma. This finding opened up the possibility of targeting this pathway with drugs to prevent bone destruction in myeloma.
Preventing myeloma bone disease
In another Blood Cancer UK-funded study, Croucher showed that a drug called zoledronic acid could prevent myeloma bone disease and the progression of the cancer itself.
Professor Croucher was joined in the lab in 2005 by Professor Andy Chantry – a haematologist who did a Blood Cancer UK-funded PhD and Clinician Scientist Fellowship. With Blood Cancer UK-funding, the team made further key advances in the understanding of myeloma bone disease.