Chronic myelomonocytic leukaemia (CMML) explained
Chronic myelomonocytic leukaemia (CMML) is a type of blood cancer that affects many types of blood cell, but white blood cells called monocytes in particular. CMML develops slowly and is a long-term (chronic) condition.
What is leukaemia?
Leukaemia is a type of cancer affecting the blood cells.
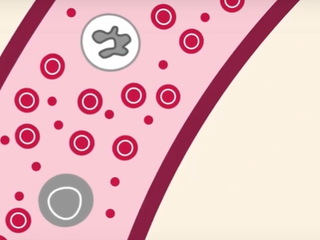
Blood cells are made inside the bone marrow, which is the soft spongy tissue found in the middle of some of our bones. The bone marrow produces stem cells, which then mature and develop over time to become different types of blood cells, such as red blood cells, white blood cells, and platelets. These blood cells play an important part in staying healthy:
- Red blood cells carry oxygen around your body.
- White blood cells help your body fight infection.
- Platelets stick together to stop you bleeding.
In leukaemia, stem cells start to make abnormal blood cells - usually it is white blood cells that are affected. These abnormal white blood cells cannot work properly to protect the body. They can also stop healthy blood cells being made.
There are different types of leukaemia. It can be fast growing (acute) or slow growing (chronic).
What is CMML?
CMML is a type of chronic leukaemia. It develops from a type of white blood cell called monocytes. Normally, these play an important part in the immune system.
In CMML, the bone marrow makes too many monocytes. They are also abnormal and do not work as they should. Over time, they may not mature properly and build up in the bone marrow. These immature monocytes are called blast cells.
Abnormal monocytes and blast cells are cancer cells (CMML cells). They cannot do their job properly and start to crowd the bone marrow, leaving little space for healthy blood cells. CMML cells can also spill out into the blood, causing leukaemia symptoms.
For most people, CMML is a long-term condition that is treatable, but not curable – it doesn’t completely go away. However, many people can have a good quality of life while living with CMML and continue to do the things they enjoy.
- Not all CMML patients need treatment straight away, and some don’t need active treatment for many years.
- When treatment is needed, it can control the cancer and put people into remission, meaning there is no sign of CMML in the body. This does not mean that CMML is cured, but it does manage the symptoms and lets people live a relatively normal life. Some people can stay in remission for a very long time.
- Some people go through cycles of remission, where there is no CMML present, followed by relapse, where the CMML returns and treatment starts again.
- A small number of people may be offered a stem cell transplant. This can cure the CMML, but it is a very strong treatment and not suitable for most people with CMML.
For many people with CMML, treatment controls the disease and the symptoms effectively. This is sometimes the main aim of treatment and can be a good outcome, allowing you to get on with your life.
Types of CMML
Understanding what kind of CMML you have can help doctors decide what kind of treatment is likely to be best for you, or even whether you need treatment at all.
MP-CMML and MD-CMML
The World Health Organisation (WHO) includes CMML in a group of blood cancers that share features with two other groups: myeloproliferative neoplasms (MPN) and myelodysplastic syndromes (MDS).
If you have an MPN, your body produces too many of one or more types of blood cell. If you have MDS, your body doesn’t produce enough blood cells. CMML has features of both and is sometimes called MDS/MPN overlap.
With CMML, you have unusually high levels of monocytes, along with high levels of other types of white blood cell. That’s like MPNs. Also, these monocytes and other white blood cells are not properly developed. That’s similar to MDS. Doctors have learnt more about CMML and been able to develop treatment for it based on their knowledge of MPN and MDS, so it’s an important connection.
CMML is seen as a separate disease that overlaps with both MPNs and MDS:
- Around half of the people with CMML produce a very large number of abnormal monocytes. This is known as MP-CMML because it is more “proliferative” like an MPN. If you have MP-CMML, your total white blood cell count (the number of white cells in your blood) will be high.
- The other half of people with CMML have high levels of abnormal monocytes, but low levels of other blood cells. This is known as MD-CMML, because it is more “dysplastic” like MDS.
CMML-1 and CMML-2
Blast cells are immature cells. Normally, you shouldn’t have any blast cells in your blood and only a few (less than 5%) in your bone marrow. But if you have CMML, you may have more blast cells than normal in both places. The level of blast cells you have may predict how quickly the CMML is likely to become more acute (faster growing).
The World Health Organisation (WHO) has classed CMML as a blood cancer with two different stages, depending on how many blast cells there are in your blood and bone marrow:
- CMML-1: less than 5% blast cells in the blood and/or less than 10% blast cells in the bone marrow
- CMML-2: from 5% to 19% blast cells in the blood and/or 10% to 19% in the bone marrow
If the blood cells in your blood or bone marrow are more than 20% blast cells, this is classed as a faster growing type of blood cancer called acute myeloid leukaemia (AML).
If CMML turns into AML, it is called transformation. About a quarter of people with CMML will develop AML at some point after their diagnosis, but it can take months or years. The chance of developing AML is higher with CMML-2 than CMML-1
What is blood cancer?
Find out how blood cancer starts and how it can affect your body and your life.
Why do people get CMML?
CMML is rare, with about 650 people diagnosed every year in the UK. It’s more common in older people – the average age at diagnosis is around 75 years old. It’s about twice as common in men than women.
We don’t know exactly what causes CMML. Research suggests that there are some things which make it more likely for someone to get it. These are known as risk factors. As well as your age and your sex, the risk factors for CMML include:
- being exposed to certain chemicals in the environment or at work
- having chemotherapy or radiotherapy treatment for cancer in the past. This is sometimes called therapy-related CMML.
- About 10% of all CMML cases (1 in every 10) are therapy related. Having therapy-related CMML may affect how your doctor treats the CMML.
For many people, there may be no clear explanation or risk factors. But we do know that developing CMML is related to changes in certain genes (genetic mutations) that typically happen as people get older.
Genetic mutations
The cells in your body contain DNA. DNA is made up of lots of different genes. These genes are like a set of instructions for each cell, telling it what to do.
Researchers think that CMML comes from changes (mutations) in certain genes which stop the cells in your bone marrow working normally.
These genetic mutations affect the blood-developing cells (stem cells) during someone’s lifetime. The reason why people develop mutations is unclear. They are not the sort of changes that can be inherited from your parents or passed on to your children.
Nearly all people with CMML have at least one genetic mutation. Many people have more than one. Here are some of the more common genes which show changes in CMML:
- TET2: seen in around 60% of people with CMML (6 out of 10)
- SRSF2: seen in around 50% of people with CMML (5 out of 10)
- AXSL1: seen in around 40% of people with CMML (4 out of 10)
- RAS: seen in around 30% of people with CMML (3 out of 10)
A third of CMML patients also have chromosome abnormalities. Chromosomes are found in the centre of every cell. They are long structures that carry DNA.
Genetic mutations are important because they can predict the risk of CMML transforming to AML and help doctors plan your treatment.

Contact our support services team
Our team of nurses and trained staff offer support and information to anyone affected by or worried about blood cancer. Contact them by phone, email, or on our Community Forum.
More About This