What is a clinical trial?
Clinical trials are an important way of developing and improving treatments for blood cancer. They also help us discover more about the causes, symptoms and side effects of blood cancer, which can lead to better treatment for everyone.
Clinical trials explained
Before any new medicine or treatment is given to people, it is tested thoroughly in a laboratory to make sure it looks safe. When experts believe it is ready, the next step is to test it in clinical trials.
The goal of most clinical trials is to find out:
- Is the new drug or treatment safe for people?
- Does it work, and is it as effective – or better – than the treatments we already have?
If a trial is successful, the new drug may become the standard treatment for everyone.
Clinical trials can also be used to:
- see if an existing approved drug or treatment for one disease can successfully treat a different disease
- test new combinations of current approved drugs or treatments
- test different ways of giving treatment, such as new medical equipment
- understand more about blood cancer and how it affects us
- learn more about symptoms and side effects, and how to manage them.
Learn about the key things you need to know about clinical trials.
Watch our video about all you need to know about clinical trials, with Urdu subtitles.
Why are clinical trials important?
Without clinical trials, we wouldn’t have any of the current known treatments for blood cancer, and it would be impossible to discover new and better treatments.
Trials can also help doctors to improve existing treatments, and reduce the risk of developing side effects and late effects.
In addition, clinical trials play a vital role in improving survival rates for people with blood cancer. In 1960 just 1 in 10 children (10%) diagnosed with the most common childhood leukaemia survived for five years after diagnosis. Today, 9 in 10 children (90%) survive.
You can read more about successful clinical trials in blood cancer elsewhere on our website, including:
- The RAPID trial, which showed the benefits of giving people with Hodgkin lymphoma body scans before and after treatment. This trial changed clinical practice worldwide and means fewer people now need radiotherapy.
- The DESTINY trial, which showed that it is possible for some people with chronic myeloid leukaemia (CML) to pause treatment, allowing them to take a break from side effects or even start a family.
- The CLARITY trial, which showed that a previously unexplored combination of drugs was a highly effective treatment for people with chronic lymphocytic leukaemia (CLL). These combined drugs were able to destroy cancer cells with fewer side effects than traditional treatment.
- The MAJIC trial, which led to a new treatment being developed and approved for polycythaemia vera (PV).
“I didn’t know anything about clinical trials at all. The first thing I ever heard about them was my nurse asking if I was interested in joining a trial. I asked for more information, and decided it was something I wanted to explore.”
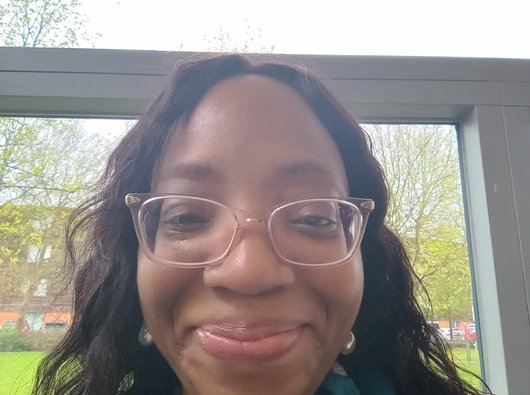
Precious, diagnosed with chronic myeloid leukaemia (CML). Read more stories from people affected by blood cancer.
Phases of a clinical trial
There are four main stages of a clinical trial, called ‘Phases’. Every clinical trial will go through these phases, and you may be invited to join a trial at any of the phases, or even more than one phase.
Phase I
Pronounced Phase "one", these trials test the safety and side effects of a new drug or treatment.
People who take part in phase I trials (up to 30 people) often have advanced cancers, and have usually tried all the existing treatment options available to them.
The first few patients to take part in a phase I trial are given a very small dose of the new drug. If they respond well, the next group have a slightly higher dose. The dose is gradually increased with each group.
The researchers monitor the effect of the drug until they find the best dose to give. This is also called a dose escalation study.
Phase II
Pronounced Phase "two", these trials test a new drug or treatment on a larger group of people (more than 100) to find out more about how exactly the treatment affects the cancer, and whether it causes any side effects.
These trials can last several weeks, months, or sometimes even years. The length of time you’ll stay on a phase II trial will depend on the blood cancer you have, whether you need short- or long-term treatment, and how successful the treatment is. You’ll be able to find out how long you might be expected to stay on a trial for before you enrol. You are also allowed to leave a trial at any time, for any reason, if you change your mind about being on one.
Phase III
Pronounced Phase "three", these trials involve more people (hundreds or thousands) and compare new drugs or treatments with the best current treatment available. Phase III trials usually last a long time, as researchers want to see how the new drugs may perform in the long term.
Phase IV
Pronounced Phase "four", these trials are carried out after a new drug has been shown to work and has been licensed to be used (a licence means the medicine can be made available on prescription).
The aim of phase IV trials is to find out how well the drug works when it’s used on even more people. Researchers also study the long-term benefits and risks, and discover more about any possible side effects.
Listen to Senior Research Nurse Tamunoibim Anidima speak to community researchers Rehab Asad and Ngozi about improving awareness of clinical trials amongst Black, Pakistani and other minoritized communities.
Listen to Senior Research Nurse Tamunoibim Anidima speak to community researchers Rehab Asad and Ngozi about improving awareness of clinical trials amongst Black, Pakistani and other minoritized communities. This video contains Urdu subtitles.
Types of clinical trial
As well as the different phases of a clinical trial, there are also different types of clinical trial. It’s important to know that whilst not every person on every type of clinical trial will receive exactly the same treatment, you will not be refused treatment if there is a suitable option available for you. You should also not be given a placebo instead of treatment, but some people may receive placebos in addition to a type of treatment. You can read more about placebos and how they’re used on our frequently asked questions page.
Open label trials
In open label trials, both you and the researchers know which treatment you’re having.
These trials usually compare two very similar treatments to test which treatment is better, and usually happen in the early phases.
Randomised clinical trials
In a randomised clinical trial, you’ll be put randomly into either:
- the treatment group – where you’ll be given the new treatment being trialled, or
- the control group – where you’ll receive the current best standard of treatment.
If you take part in a randomised trial (most phase III and some phase II trials are randomised) a computer programme is usually used to randomly select which group you will be in. Your personal details, such as your age, gender and general health are all taken into account so that the groups in the trial are as similar as possible. This helps to make sure that the results of the trial are reliable and accurate.
Blind clinical trials
A blind trial is a trial where the people taking part don’t know which treatment they are getting. You might get the new treatment. Or you could receive the current standard treatment.
So that nobody can tell which treatment they are having, everyone taking part will receive identical looking injections, tablets, or other forms of treatment.
Double blind clinical trials
In a double blind trial, you won’t know if you’re getting the new treatment or the current standard treatment, and neither will the researchers, until the end of the trial.
This makes sure that the results are more reliable as they will not be influenced by your expectations or the researchers’ expectations.
How clinical trials are funded and planned
Clinical trials in the UK are mainly funded by the government, drug companies (also called pharmaceutical companies), and charities.
All trials, no matter who funds them, are checked and monitored in similar ways to make sure that everyone involved is protected from harm.
Each trial also has a sponsor who is responsible for running the trial. The sponsor may be the organisation funding the trial, or the institution leading the research (for example, a university or a hospital).
Once a group of researchers have an idea for what they want to test in a trial, they need to develop a protocol.
A protocol is a detailed plan for the trial, which includes:
- why the trial should be done
- the number of people involved
- who should be able to take part in the trial (this is called the eligibility criteria)
- details of the treatments given in the trial
- what medical tests people will have and when.
Everyone involved in a trial must use the protocol. This keeps everyone taking part safe, and makes sure that the results of the trial can be trusted.
Are clinical trials safe?
Lots of people say that one of the biggest worries about joining a clinical trial is being used as a “guinea pig”. The word “trial” can also be off-putting, as you may be concerned that doctors and researchers don’t know how safe a drug or treatment is before testing it.
New drugs and treatments are tested extensively in a laboratory before being given to humans, and there are strict regulations in place to make sure that a drug is safe before it reaches any phase of clinical trial.
We know that safety and honesty were not always prioritized on some clinical trials in the past, and that this has understandably led to mistrust or doubt amongst some communities. Thankfully, strict guidelines, rules and regulations now in place ensure clinical trials are safe and ethical for everyone involved. Trials in the UK today are closely monitored by the following groups:
Medicines and Healthcare products Regulatory Agency (MHRA)
The MHRA is a group of the Department of Health, that makes sure the safety and quality of the treatment tested in a trial meets good practice standards.
There are strict rules in the UK to keep people safe and protect personal information, and studies involving medicines need extra checks from the MHRA.
Research ethics committees
Before any trial involving people can begin, it’s reviewed by an independent Research Ethics Committee (REC) to make sure it’s fair, respectful, and protects everyone taking part.
Research Ethics Committees are groups run by the NHS Health Research Authority. They are independent groups of people including doctors, nurses, other medical staff, members of the public and sometimes lawyers.
An Ethics Committee also makes sure that the information you are given tells you everything you need to know, and is easy to understand.
The Health Research Authority
The Health Research Authority (HRA) is a public body that protects and promotes the interests of patients and the public in health research, such as trials. Their involvement helps to ensure that all information about a trial is clear, that potential risks are spotted, and that the research meets real needs.
Clinical trial committees
These are national and local groups in your hospital or research centre that make sure that the trial is planned well and carried out safely.
They also check that the trial is based on scientific knowledge and follows national guidelines and safe practices.
It may also help to know that you will only be allowed to join a clinical trial if your doctor believes that the benefits outweigh any risks, and if you are a suitable candidate for the new treatment – this is called your eligibility.
Even if you do join a trial, if you or your doctors feel at any point that it is no longer right for you, you can leave it. This will not affect any alternative care you may be offered.
PVGAN (Patient Voice Grant Advisory Network)
At Blood Cancer UK, we make sure that any research we fund - like laboratory studies or grants - focuses on what matters most to people affected by blood cancer.
We do this through our Patient Voice Grant Advisory Network (PVGAN), where people with lived experience review research ideas and materials to check they are clear and relevant. It’s just one way we make sure our funded research is shaped by real experiences and builds trust.
Consent
Consent is when you give your permission to have any medical treatment, test or examination.
If you are invited to join a clinical trial, a member of the research team will tell you what to expect and what the trial hopes to achieve. They will provide you with all the information you need to make a decision about whether you want to take part in the trial, and answer any questions you or your loved ones may have.
You should also be given a patient information sheet by the organisers of the trial, which contains detailed information about the trial, the researchers, the funding, and who to contact if you want to find out more.
Understanding the complex information needed to enrol on a trial can be overwhelming, but our Clinical Trials Support Service is here to help you navigate through the entire process – whether you're a patient, carer or the loved one of someone affected by blood cancer.
Once you have decided to take part in a clinical trial, you’ll have to give your informed consent and sign some forms. These forms are important legal documents that protect both yourself and the organisation running the trial.
Remember, even if you do join a clinical trial, you can leave at any point if you change your mind. We have some more information on what happens when you leave a clinical trial.
You may wish to discuss alternative treatments with your doctor, or ask them what will happen if you don’t join the trial, so that you understand all of the options before making your choice. We’ve listed some questions you might want to ask on another page.
Accessing your data
The NHS and the trial sponsor (the organisation running the study) have strict confidentiality rules about who can and can’t view your information. Only the clinical and research teams who need to access your records will be able to see them.
Before you give consent to join a clinical trial, the researchers will explain what personal data they need to record and access, and why. You will have the chance to ask questions at this stage.
Once you’ve agreed to take part in a trial, you’ll be given a trial number to make sure your information is kept anonymous. If your information needs to be sent out of the hospital, the trial team will use this number, and all of your personal details will stay in your notes.
About our health information
This information about clinical trials is accredited with the PIF TICK, the UK's only quality mark for trusted health information.
Last full review December 2025. Next full review due December 2028. We may make factual updates to the information between reviews.
We would like to thank Consultant Haematologist Dr Priya Sriskandarajah for checking the clinical accuracy of this information. Thank you also to everyone who participated in the community research for this project, and shared their experience of clinical trials.

Worried about anything or have questions?
If you need someone to talk to, please don't hesitate to contact our Support Service by phone or email.
