Blood cancer and infection
What you need to know:
- You may be at higher risk of infection if you have blood cancer.
- People on active treatment are at particularly high risk.
- Your hospital team can tell you about your personal risk of infection and what you can do to help.
What causes infection?
Infection is caused by bacteria, viruses, fungi and other harmful microbes commonly known as germs.
Most germs aren’t harmful, but some can multiply inside our bodies and start to cause damage.
Normally, our immune system protects us against germs. But blood cancer and blood cancer treatment can weaken the immune system. So infections can happen more often, last longer and become more serious than normal.
Infection and sepsis
If an infection isn’t spotted and treated, it can develop into sepsis. This happens when your body overreacts to infection, and it can be very serious.
It’s important to know that you may be at higher risk of infection and sepsis if you have blood cancer.
We have information about what to look out for and what to do if you think you have an infection.
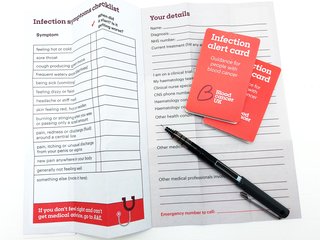
Order your free infection alert cards
With our pocket guide you can record infection symptoms and personal details to share with medical staff. Find out what to do and what to say if you go to A&E.
It's like peak covid
”It's a bit like going back to life as if it was peak covid. Handwashing, using anti-bacterial wipes, hand sanitiser, wearing facemasks, social distancing. All these things can help when you're at high risk.”
Ritesh, diagnosed with Hodgkin lymphoma in 2022

Am I at risk of infection?
The simple answer is yes, if you have blood cancer. But the level of risk varies from person to person. It will depend on how the cancer affects your immune system, what treatment you’re having, and any other health conditions you may have.
You are at highest risk of infection if:
- You are neutropenic – you have a low level of white blood cells called neutrophils.
- You are having any treatment for blood cancer, including chemotherapy, targeted therapies, steroids, radiotherapy, stem cell transplant or CAR-T therapy.
- You are taking immunosuppressant drugs, such as steroids or ciclosporin, for another condition. (These drugs stop the immune system attacking healthy cells but also affect how it fights infection.)
- You have had your spleen removed or have problems with your spleen, an organ which is part of your immune system.
- You have a central line fitted, making a small wound where the line breaks the skin.
- You have a sore mouth or mouth ulcers (mucositis) as a side effect of treatment.
- You have broken skin because of a rash or itching, a side effect of some blood cancers or treatment.
Your hospital team may give you antibiotics while you’re being treated just in case you get an infection. These are called prophylactic antibiotics.
They will lower your risk of infection but won’t necessarily stop you getting one. Also, they won’t treat an infection once you have it. So it’s important to be aware of infection and get help if you notice any symptoms.
If you are not currently having blood cancer treatment, your risk of infection may still be higher than normal. Think about whether you have infections more often than you used to, and whether they take longer to go.
Ask your consultant or clinical nurse specialist (CNS) about your personal level of risk.
Ask questions and get all the information you can
”When you come off chemo or a line of treatment, and it's been effective, it feels like you're left to your own devices for a long time. And that is the time really when you need to have a clear view of what to watch out for.
So you should be getting a clear idea about your level of infection risk after treatment as well. If you don't get that, you should ask. The more information you have, the better able you are to make decisions about how you live your life.”
Mat, diagnosed with myeloma in 2017

What to ask your hospital team
Here are some questions you may want to ask your team:
- How is the blood cancer affecting my immune system?
- Am I neutropenic? (new-tro-pee-nick)
- What do I do if I think I have an infection?
- Is my risk of infection higher than normal?
- Do I need to make changes to protect myself?
- Will the treatment put me at risk of infection?
- What can I do to protect myself?
- When can I stop taking extra precautions?
- Is my immune system back to normal?
- Do I still need to protect myself against infection?
- Are there any activities I should avoid?
Why covid was an eye-opener for me
“When I was diagnosed with AML, I was given information about neutropenia and told the chemotherapy would completely destroy my immune system. So that was all managed very well whilst I was going through treatment.
But when covid struck, I was actually quite shocked that I was told to shield. I hadn't really appreciated that I should be taking more care than the average person to reduce my risk of catching some kind of respiratory condition.
Now I feel safer knowing that I've had multiple vaccinations, but the risk of infection is always at the back of my mind.”
Jane, diagnosed with acute myeloid leukaemia (AML) in 2014.

How does my body fight infection?
Your immune system is a network of cells, tissues and organs which protects your body against infection. Your white blood cells play an important role in this.
The main white blood cells which fight infection are lymphocytes and neutrophils. They work in different ways to find and destroy germs that could be harmful.
If you have low levels of white blood cells, your body will find it much harder to fight off infections.
A low level of neutrophils is called neutropenia. Neutropenia is a common side effect of some blood cancer treatments.
If you have neutropenia, you are at particularly high risk of infection and sepsis, which can be dangerous. So you may need to be more careful about managing your infection risk while you are neutropenic.
We have more information about how blood cancer affects your immune system.
