Because my journey can help someone with theirs
It's been four and a half years since Jane achieved remission. Here, she reflects on the painful symptoms and "horrible" side effects of her blood cancer treatment, and explains that without taking part in a clinical trial, she wouldn't be here today.

I was diagnosed with acute myeloid leukaemia in December 2014. In the months leading up to my diagnosis, I had a bad cold, sinusitis and conjunctivitis. I even had two rounds of antibiotics for gum pain, which didn’t help at all! I developed a rash all over my body and my face became very swollen.
I went to the doctors and gave blood samples. That evening, my doctor called and told me to go to the hospital, where I was diagnosed. I never imagined it would be as serious as leukaemia.
All I knew about the disease is that people can die from it. I was pretty terrified.
Three cycles instead of four? Sign me up!
Due to the type of leukaemia I had, my consultant suggested that I take part in the AML17 clinical trial. This meant I had a 50/50 chance of having just three cycles of chemotherapy instead of four. I signed up straight away.

My final cycle was fraught with problems
I developed an infection, where the source was unknown for some time. I was given numerous antibiotics, which failed to clear it up and I was in a lot of pain.
It turned out to be an infected fallopian tube. After 11 weeks in hospital, I was finally discharged. Finally, in April 2015, I was told that I was in remission.
The feeling was absolutely amazing! I thought that was it, the whole ordeal was done.
Although the worst was over, I still felt very weak, but I was home and with my family.
The side effects of chemotherapy are awful. The worst of it was having painful sores that made it incredibly difficult to eat or swallow. I had absolutely no energy or immune system and developed horrible infections and side effects.
The clinical trial
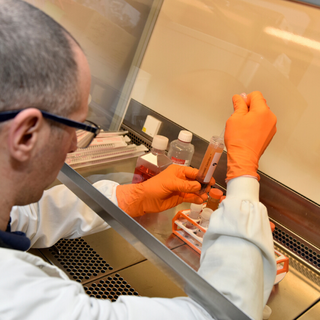
As part of the clinical trial I was on, called AML17, I had additional monitoring for minimal residual disease (MRD). This meant I had a bone marrow biopsy every three months for a further two years following remission. This part of the clinical trial was funded by Blood Cancer UK.
The minimal residual disease test
Our researchers created the first minimal residual disease (MRD) test that detects cancer cells that are left behind in the blood or bone marrow after treatment.
This test is used worldwide and can tell you how someone has responded to their initial treatment. This helps doctors to plan the intensity of subsequent treatment.
A few days after my first bone marrow biopsy, I was back in hospital for a keyhole surgery to remove the infected fallopian tube. Before the procedure, I was asked to do another bone marrow biopsy.
They didn’t say anything at the time, but it was clear that something was wrong. I was so worried. While recovering from surgery, I was told that the leukaemia had returned. It was such a huge blow, and I was absolutely devastated.
I’m incredibly lucky to have been part of the clinical trial and to have found this out then.
Back on treatment
I had three cycles of chemotherapy and tried a new combination of chemotherapy drugs, which unfortunately didn’t work. Thankfully, I was able to have an experimental American drug, which showed a lot of promise in a small-scale clinical trial.
It was available in the UK, but only privately. Luckily, I had private medical insurance, and my employers agreed to fund two cycles.
This was so much better than chemotherapy. I had far fewer side effects and got back into remission in February 2016.
My stem cell transplant
I was told that I needed to have a stem cell transplant to reduce the risk of my cancer returning. Fortunately, my sister was a match, but her body mass index was too high. While I was on treatment, she lost three and half stone. I’m really proud of her.
Without being on the clinical trial, and specifically part of the trial that Blood Cancer UK funded, I wouldn’t be here today.
I’ve learned, first-hand, about the benefits of clinical trials and there are always new ones taking place. I had a pretty horrendous treatment journey, but I hope that by taking part in the clinical trial, someone else will have a better experience – with fewer side effects and a better chance of survival.

Contact our Clinical Trials Support Service
Get personalised support to understand which clinical trials are available - whether you're a patient, carer or healthcare professional.