Facts and information about blood cancer
Blood cancer is the UK’s third biggest cancer killer, and yet awareness and understanding of it is much lower than for other types of cancer.
What is blood cancer?
Blood cancer is a type of cancer that affects your blood cells, and includes leukaemia, lymphoma, myeloma, myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN), including essential thrombocythaemia (ET), polycythaemia vera (PV) and myelofibrosis.
Blood cancer is what happens when something goes wrong with the DNA in your blood cells. These blood cells become abnormal, and multiply. These abnormal cells do not work properly, and so your blood is less able to carry out its role in keeping your body healthy, such as by fighting off infections or helping to repair your body.
Find more information on this in our what is blood cancer section.
How common is blood cancer?
Blood cancer is the fifth most common cancer in the UK, with over 40,000 people being diagnosed with it every year.
There are about 250,000* people living with blood cancer in the UK. One in every 16 men and one in every 22 women will develop it at some point in their lives.
It is the most common type of childhood cancer. Every year, more than 500 children aged under 15 are diagnosed with blood cancer. Of these, about 400 have childhood leukaemia and about 100 have lymphoma.
The risk of blood cancer goes up as you get older, and just under 40% of people diagnosed with it are aged 75 or over.
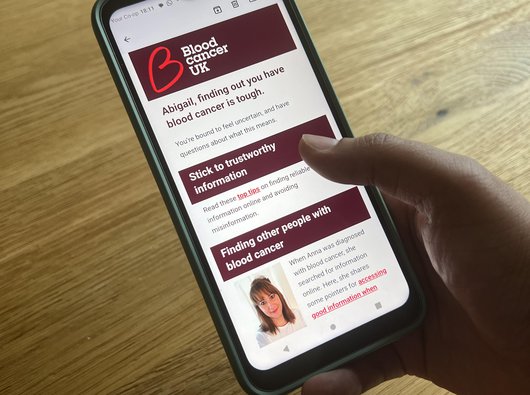
If you've just been told you have blood cancer
Sign up to our weekly support email for people recently diagnosed.
It gives you clear and simple information, practical tips and advice from others with blood cancer, to help during the first few weeks and months after diagnosis.
Different types of blood cancer
There are more than 100 different types of blood cancer. Most of these are types of leukaemia, lymphoma and myeloma, but the term “blood cancer” also includes other conditions such as myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN).
Some are fast growing (these types of blood cancer are called “acute”), while others grow more slowly (chronic). Sometimes the type of blood cancer can change as cancer develops. For example, MDS can turn into acute myeloid leukaemia (AML).
The five most common types of blood cancer are:
- Diffuse large B-cell lymphoma (affects 5,500 people a year)
- Chronic lymphocytic leukaemia, or CLL (affects 4,700 people a year)
- Myeloma (affects 4,500 people a year)
- Chronic myeloproliferative neoplasms (MPNs) (affect 3,900 people a year)
- Marginal zone lymphoma (affects 2,700 people a year)
- Acute myeloid leukaemia, or AML (affects 2,700 people a year)
There is more information about the different types of blood cancer in our understanding blood cancer section.Acute myeloid leukaemia (AML)
How many people die of blood cancer?
Blood cancer is the UK’s third biggest cancer killer, and every year about 16,000 people die of it.
Overall, the five-year survival rate for blood cancer is around 70%. That means someone diagnosed with blood cancer is only 70% as likely to be alive in five years as someone their age who doesn’t have cancer.
But while 70% is an overall average for all types of blood cancer, different types have very different survival rates.
Research breakthroughs over the last few decades mean that the five-year survival rates for chronic myeloid leukaemia (CML), chronic lymphocytic leukaemia (CLL) and follicular lymphoma are over 85%. But with acute myeloid leukaemia (AML), mantle cell lymphoma and myeloma, the five-year survival rate is less than 50%.
It is important to understand that these are also averages, based on what has happened to a large group of people, who all survive for different lengths of time. An individual person’s chance of a good outcome will depend on lots of factors. Even two people with the same condition can have quite different outcomes. So try to listen to what your clinician tells you about your prognosis, rather than worrying too much about overall survival rates for your type of blood cancer.
How has blood cancer survival changed over time?
We have come a huge way since Blood Cancer UK was founded in 1960. Back then, just one in 10 children diagnosed with the most common type of leukaemia survived. Today, nine in 10 children survive. And this has continued, with new treatments being developed every year and survival rates for blood cancer increasing faster than for other cancers.
You can find out more about the impact of the £500 million we’ve invested in research since 1960 on our research impact page.
But there is still a long way to go before we get to the point where everyone with blood cancer survives. Find out how you can fundraise to help us get there.
NHS treatment for people with blood cancer
Every year, the NHS gives world class treatment to many thousands of people with blood cancer. But there are still areas where the NHS could be doing better:
- Just 67% of people with blood cancer only have to see their GP once or twice before being diagnosed. This compares to 94% for breast cancer, and 82% for prostate cancer. This is a serious issue because the sooner you are diagnosed, the better your chances of treatment being successful.
- When they are diagnosed, just 60% of people with blood cancer completely understand what is wrong with them. This is much lower than for breast cancer (77%); prostate cancer (79%); or lung cancer (76%). This is why we produce health information to help people understand their type of blood cancer.
- Just 33% of people with blood cancer are spoken to about taking part in cancer research. That’s about the same as for breast, lung or prostate cancer, but we think it is too low, because taking part in a trial can mean getting access to a promising new treatment not yet available on the NHS. You can talk to us and get information about any suitable trials by using our clinical trials service.
A big part of our work involves campaigning for improvements to healthcare for people with blood cancer. Find out how you can support our campaigns.
There are more than 200,000 people with blood cancer in the UK who are “clinically extremely vulnerable” to the coronavirus and, so have been advised to take particular care to avoid coming into contact with the virus.
A study published at the end of 2020 looked at what happened to 3,377 people with blood cancer across the world who contracted the coronavirus. It found that 34% died, compared with 22% of people who did not have blood cancer and were in hospital with the coronavirus. This means that among hospital patients, it appears that people with blood cancer are about 50% more likely to die from coronavirus than someone who does not have blood cancer.
But the real chance of dying if you have blood cancer and get coronavirus is likely to be lower than that, because the study mostly looked at people with blood cancer and coronavirus in hospital. We don’t know how many people with blood cancer have had coronavirus without symptoms, or have had coronavirus but weren’t ill enough to need hospital treatment.
As well as being at higher risk from the virus, avoiding the virus has led to a huge mental health impact for people affected by blood cancer.
In May 2020, we conducted a survey of 1,077 people affected by blood cancer that found that over half of people with blood cancer were struggling with their mental health. Almost one in 10 said the impact was severe.
It also found that three quarters (75%) of the 605 friends and family members who took part in the survey said that supporting a person with blood cancer during the pandemic had increased their levels of stress.
*There are now approximately 280,000 people living with blood cancer in the UK. (Figure accurate as of February 2025).
