The blood cancer jigsaw: how we start to piece together the bigger picture
There are many different types of blood cancer, which affect different blood cells and require different treatments. But blood cancers might be more similar than you think – in this blog we look at what ties them together, the similarities between treatments, and how some drugs and research are having an impact across multiple conditions.
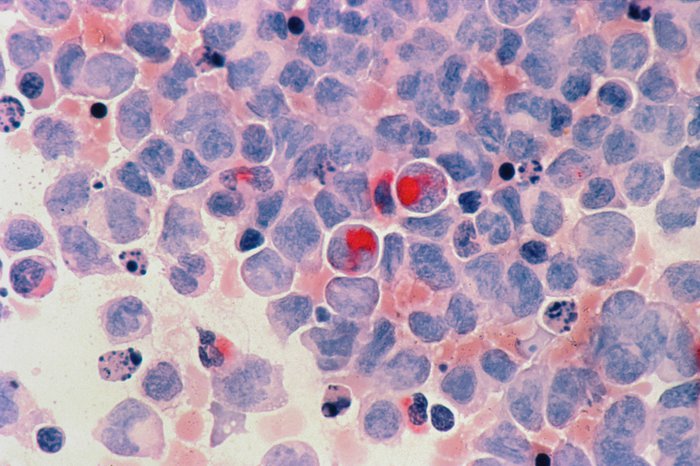
Acute myeloid leukaemia cells under the microscope
Cancer – a disease of cells growing uncontrollably
In its simplest form, cancer is defined as a ‘disease where abnormal cells grow uncontrollably’ [1]. Most (if not all) cancer cells have a handful of similar ‘bad’ characteristics [2]. For example, most healthy cells have a self-destruct button when things go wrong but cancer cells can ignore these signals, carry on growing uncontrollably, and spread to other areas of the body where they shouldn’t be.
There are many factors which link cancer cells generally, but blood cancers are even more connected.
How are blood cancers broken down into categories?
There are over 100 different types of blood cancer and related conditions [3]. Most commonly they are grouped by the location they were first detected: in the blood (leukaemias), lymph nodes (lymphomas) or bone marrow (myelomas).
This is how you’ll likely see blood cancers grouped and recorded in national statistics, but our understanding of blood cancers and pre-cancerous conditions has changed significantly in recent years and so classifying blood cancers based on where they are detected is no longer as useful as it once was thought to be. Perhaps unsurprisingly, its more complicated.
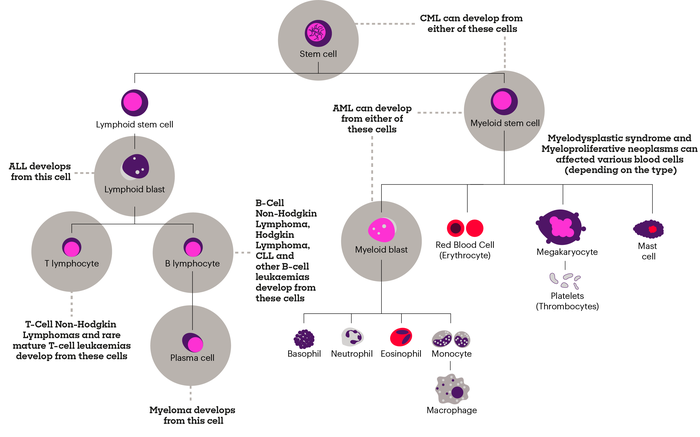
Blood cancers can be connected by the cell they arise from
Today we have a far better understanding of how blood cancers are connected. All blood cells develop from one type of ‘blood stem cell’ called a haematopoietic stem cell. It takes many steps to create all the different blood cells in our bodies, which unfortunately means there are many steps in which things can go wrong.
Take chronic lymphocytic leukaemia (CLL) for example.
CLL is actually more closely related to some types of lymphoma as opposed to other types of leukaemia because CLL and some lymphomas arise when something goes wrong in a B-lymphocyte. Whereas in chronic myeloid leukaemia (CML) it’s a completely different type of blood cell called a granulocyte that turns cancerous.
Understanding this further means researchers can now start to pinpoint the step at which something goes wrong and causes blood cancer to develop.
Similar cancers mean similar treatments
Because of their similarities, there are many common treatments used across different types of blood cancer. Chemotherapy and stem cell transplants and two common treatment approaches but in recent years there has been a new wave of treatments.
Imatinib (originally branded as Gleevec) is a tyrosine kinase inhibitor (TKI), that was first licenced in the US to treat chronic myeloid leukaemia (CML) in 2001. Today it is used to treat several leukaemia’s (including CML and ALL), myelodysplastic syndromes, myeloproliferative neoplasms, as well as some gastrointestinal tumours. Imatinib transformed CML from a relatively rare but fatal disease (in those who did not have a transplant), to a long-term and potentially curable condition.
Rituximab is another example. It is a targeted cancer drug called a monoclonal antibody, which today is used to treat multiple blood cancers.
Rituximab was first licenced for use in the US in 1997 to treat B-cell non-Hodgkin lymphoma that was resistant to other chemotherapy regimens. Today it is approved for use in the UK to treat chronic lymphocytic leukaemia (CLL) and some types of non-Hodgkin lymphoma.
Bortezomib is a third example used to treat myeloma. Although myeloma results from several mutations, that differ from person to person, the cells share a common link which makes Bortezomib effective for many people with the disease.
This drug, which is called proteasome inhibitor, stops the cell from trying to fix faulty proteins created due to the ‘cancerous nature’ of the cell, meaning the cancer cell is destroyed. This drug is now used in both myeloma and mantle cell lymphoma, as the same mechanism can be targeted in both disease.
All these examples show that there are common targetable pathways across multiple blood cancers.
But aren’t we trying to make treatments more personalised?
Despite their similarities, huge efforts are being made to make treatments more personalised and specific to an individual’s condition. But even these more ‘personalised approaches’ have had an impact across multiple blood cancers.
CAR-T therapy, a poster child for personalised approaches because it uses the individual’s own cells, was first approved in the US in 2017 to treat B-cell acute lymphoblastic leukaemia (B-ALL), but is now also used to treat certain types of non-Hodgkin lymphoma and more recently myeloma (in the US).
While scientists try and make treatment more personalised, looking at tackling the nuances between patients diagnosed with, on the face of it, the same type of blood cancer, we mustn’t forget to look for the similarities between blood cancers and how the development of new treatments might have the potential to be used for several blood cancers.
Ultimately there needs to be a balance between ‘precision medicine’ and finding common weaknesses across several blood cancers.
There’s been lots of progress made, but still lots more to be done
There has been a lot of progress in blood cancer treatment and survival, thanks to research. For example, in 1971 people diagnosed with leukaemia (average across all types) had a 13% chance of surviving 5 years, but in 2016 this was 62% [4].
As part of our plan for the future, Blood Cancer UK has made a commitment to fund research which looks at the ‘similarities’ and highlights the links across blood cancers.
Because we are Blood Cancer UK, and we will beat blood cancer within a generation.
Because research will beat blood cancer
Over 60 years, we've invested more than £500 million in blood cancer research which has led to a long line of breakthroughs that have improved treatments and saved lives.
Footnotes:
- World Health Organisation cancer definition - https://www.who.int/health-topics/cancer#tab=tab_1
- Hallmarks of cancer: the next generation, by Douglas Hanahan and Robert A Weinberg, https://pubmed.ncbi.nlm.nih.gov/21376230/
- Facts and information about blood cancer- https://bloodcancer.org.uk/news/blood-cancer-facts/#:~:text=There%20are%20over%20100%20different,are%20much%20less%20well%2Dknown
- HMRN - https://hmrn.org/statistics/quickstats
