What effect is COVID-19 having on blood cancer research?
United Kingdom
One of the questions I’ve been asked most often since the UK entered lockdown is “what does COVID-19 mean for blood cancer research?”. After two months of lockdown, what have we learned? What does the future hold and what part will Blood Cancer UK play?
A sudden shock to the system
From the point that lockdown began, medical research across the UK has been dramatically affected. At Blood Cancer UK, the vast majority of the research we fund is conducted in laboratories or involves people with blood cancer who are taking part in clinical trials. Social distancing rules and restrictions on travel meant that research conducted in laboratories had to stop very quickly. And work on clinical trials very quickly slowed down or stopped completely, because the NHS needed doctors and research nurses who usually ran trials to care for people with COVID-19.
A journey with no map
Just like the rest of us, the research community hasn’t experienced anything like this. In nearly thirty years in research I’ve seen some awful setbacks. Individual scientists and even whole departments struck by disasters, like years of research being destroyed by fire, or critical equipment failures. But COVID-19 has touched every scientist in the country. Everyone has begun a journey with no map, making the best decisions they can on limited evidence (something scientists really hate), and facing a future dominated by uncertainty. It’s an anxious and uncomfortable time, but one in which every research team is going the extra mile to make a difference.
Clinical trials – a pause with consequences
Clinical trials are a critical part of blood cancer research, and something the UK is very good at. These are the careful studies where some patients are given the best treatment currently available and others are given a new and promising treatment. By looking at what happens to each set of patients, scientists can then compare the results and see if the new treatment is better.
Trials aren’t just important for the people who will benefit from new treatments in the future – they also provide “last chance” access to experimental treatments for people who have stopped responding to the drugs we have available today. Some of the trials I’m proud that Blood Cancer UK has funded have been the only ones available for people with particular types of blood cancer. And in only five years at Blood Cancer UK I’ve seen PET scans introduced to see if people with Hodgkin lymphoma can avoid the need for radiotherapy, a key new test to show if treatment is working for some patients with acute myeloid leukaemia (AML), and hope that some people with chronic myeloid leukaemia (CML) could stop taking treatment completely.
So, pressing “pause” on clinical trials was a very difficult step for the country to take. It happened for two reasons. First, because most of the clinical staff who normally run trials were needed for the COVID-19 response. And second, because normal blood cancer treatment has changed, to reduce the chances of catching COVID-19, and to avoid treatments that suppress the immune system and may make it harder for people with blood cancer to fight COVID-19 if they catch it. For patients already on trials, doctors have worked to maintain treatment wherever this could be done safely. But most trials have been unable to recruit new patients, so, tragically, it’s likely that some of people with blood cancer will now die sooner, when taking part in a trial may have given them a longer life.
I also worry about the long-term effect on blood cancer trials, but it is still hard to say how much damage has been done. At best, the results of many trials will be delayed. Some of the data collected from some patients on trials will be incomplete and the results may tell us less about how drugs work than we had hoped. Or we may need to add more patients to studies, which comes at an added cost. It is possible too that some trials may no longer be viable and may not restart. If this is because time has moved on and better treatments are available in new trials, then that is OK. But if important trials can’t restart – or limp along slowly and at great expense – that would be hugely damaging.
Restarting clinical trials – an urgent challenge, with opportunity
The good news is that Government bodies are already developing plans to restart trials, and Blood Cancer UK, along with other medical research funders, has been consulted on new guidance from the English National Institute for Health Research.
But the road ahead is long and may be frustratingly slow. If we restart trials, we need to make sure we don’t then have to stop them again if there’s a second wave of the virus. So careful steps will need to be taken to prioritise which trials start first, and make sure all the resources they need are in place. A key part of our work over the next few months will be making sure that the trials we fund can re-open. But restarting trials is extra work that comes at a price, and there may be further additional costs for some trials if results have been lost during the shutdown and need to be repeated. These are all costs that I fear charitable funders may not be able to bear alone at a time when their income is severely affected.
As bad as the pause to clinical trials has been, necessity is the mother of invention and there have been some positive changes for some patients with blood cancer. Now the challenge is to take the best of these and hold on to them.
Access to some newer treatments that aren’t yet funded on the NHS has been widened by the NHS in England and other countries. This was done to give doctors more treatments options that can be delivered to patients at home, and that are less immunosuppressive, so are less likely to reduce a patient’s ability to fight off a COVID-19 infection. It has given doctors more and sometimes better options for treating their patients. These are temporary measures – but if these drugs are safe to use now, do we need to go back to “normal” or is now the time to find quicker ways to test the value of new treatments for the NHS?
Across the world, regulatory agencies have changed their approach to trials, allowing fewer visits to hospitals for checks by doing more of their checks over the phone or video-conference and delivering more of the drugs to people at their homes. Again, these are temporary measures. But doctors and regulators have known for years that the bureaucracy that’s there to keep patients in trials safe is in fact making trials inconvenient for patients and slower and more expensive to deliver. I think we can learn from what’s happened over the last few months so that we can have a new way of doing clinical trials that makes them cheaper and less intrusive for the people involved.
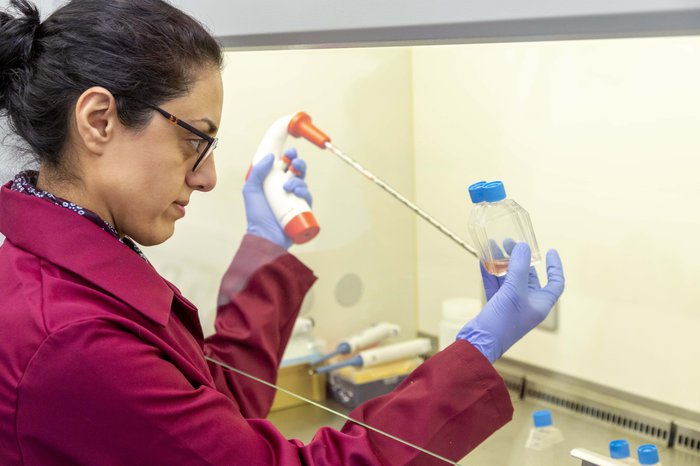
How laboratory research has changed
Clinical trials are vital for finding out whether new treatments work, but they couldn’t happen without the laboratory research that produces new tests and treatments, and then tells us how they actually work in people.
Research laboratories never normally close and shutting down labs is about much more than turning off the computer and lights and making sure the doors are locked. Blood cancer research usually involves working with cell samples donated by people with blood cancer, and where research questions can’t be answered in humans, sometimes it means working with animals. Both need long-term planning and daily attention, 365 days a year. Even planning a holiday with a scientist is a nightmare, as they barter with colleagues to look after their experiments - so having everyone stop all their work at the same time is a huge problem.
Laboratory research also depends on specialist equipment and chemicals that scientists use in their experiments. This is where COVID-19 has had some very specific effects on laboratories. Many laboratories have loaned core equipment and reagents that are useful to the national COVID-19 testing effort. That’s helping us all confront COVID-19, but it all happened very quickly - I’ve even heard of one quick-witted haematologist who had to rescue a key piece of equipment they need to keep providing important tests to patients in a trial. Thankfully those stories are few and far between. But getting equipment back and working will produce challenges as laboratories begin to return to work.
Once laboratories were closed, research teams needed to find new ways of working. Like many workers, videoconferencing has helped teams continue to work together – some of our scientists have even run virtual “lab tours” for our supporters. But what does work look like when experiments can’t continue? In the short-term, this means time to analyse data from experiments, write up research for publication and plan new work. And many labs tell us that has been a real benefit, as it is normally hard to set aside time for this work. But there’s only so long many members of research teams can productively work in this way before they run out of things to do.
How Blood Cancer UK is responding to the challenge
All of the research we fund depends on the support we receive from the public – and COVID-19 has had a large effect on our income. So that means we have less money to spend on research at a time when we would ideally spend more.
Our immediate response to COVID-19 was to focus our effort on providing certainty to the research teams who currently receive funding from us. For most of our awards that means allowing research grants to stay open longer, but at no additional cost to us. To maximise the cost savings labs can make we teamed up with other medical research charities to make sure that the government’s job protection scheme could be used to furlough charity-funded research staff, then encourage universities to make use of the scheme. Doing this will give the research we fund the best chance to restart and recover.
Now, my focus is on maximising the amount of money we invest in new blood cancer research. We expect to spend £1.8m less on research this year than we had planned unless we can make up the shortfall we expect in our income. This means good research will go unfunded, and I fear that some good young researchers may leave and not return – and who can predict how many breakthroughs won’t come to pass over the next ten or twenty years if that happens? To make choices which are affordable and have the greatest chance of changing lives for patients we will delay most of our funding decisions to the end of the year as by then we’ll have a better idea of how much we’ll be able to spend. But what then?
Given all this, I’m worried about the future. We’re just beginning work on a new research strategy that will set out the opportunity for blood cancer research in the UK. But if we can’t fund as much research, then we’ll make fewer breakthroughs and this, in turn, would mean fewer new treatments. It could mean that thousands more lives will be lost before we finally reach the day when no one dies from blood cancer.
But the really important point is that this is not inevitable. The more money we can raise to plug that £1.8 million funding gap, the less bad the impact on research will be. This means we’re relying on our community more now than we’ve ever done before.
This is the thing that gives me comfort
Over the last 60 years our community has defied the odds again and again, as we’ve gone from operating out of a kitchen in Middlesbrough to funding £500 million of research that’s transformed blood cancer care. I’ve seen first-hand the generosity, determination and ingenuity of our community.
So yes, the odds against us keeping our dream of beating blood cancer on track are long. But there isn’t a group of people I’d rather be facing those odds with than our community.

Sign up to our enewsletter to stay updated on our progress
Join our mailing list to keep updated about the latest news, research, and the ways you can help – including campaigns and events that you might be interested in.
