Types of treatment for follicular lymphoma
Treatment for follicular lymphoma can include immunotherapy, chemotherapy, radiotherapy, and combinations of different types of treatment. This page contains more detail about the treatment you may have and what to expect from your appointments.
Key things to know
- There are lots of types of treatment for follicular lymphoma, and more are being developed all the time. Current options include immunotherapy, chemotherapy, radiotherapy and combinations of different treatments.
- If you need treatment, your doctor will look at things like your symptoms, how much of your body is affected by the lymphoma, and the size of any lumps you have. This will help them decide which treatment to recommend for you.
- If the lymphoma comes back after treatment, you should be able to have more treatment. This might include joining a clinical trial.
What will treatment look like?
How much treatment you have and what type of treatment you need will depend on things like:
- your age and overall health
- the location of any swollen lymph nodes (lumps)
- how many lumps there are
- the size of the lumps
- any other symptoms you have.
We explain more about the different types of treatment that are currently available in the UK further down this page.
Treatment for follicular lymphoma can be intense and time consuming, and most people end up needing to take a break from work or studying. If you’re worried about this, or have any financial concerns, our money and work page might help. We also have more information for family and friends, including how they can support you through treatment.
If you get any side effects from treatment and find them too difficult to manage, speak to your GP or hospital team – they may be able to suggest things to help.
First line treatment
The first round of treatment you have is called first line treatment. The aim of first line treatment is to reduce the number of lymphoma cells in your body as much as possible.
The most common first line treatments for follicular lymphoma are chemo-immunotherapy, immunotherapy on its own (called single line immunotherapy), and radiotherapy. Some people might have just one of these treatment types, and others may need more than one type.
Chemo-immunotherapy
Chemo-immunotherapy is a combination of immunotherapy and chemotherapy drugs. You might also hear it named immuno-chemotherapy. It is usually given as a liquid through a needle in your arm, and it can take a few hours for each infusion to complete. You can read more about what to expect from your appointments further down this page.
We also explain more about immunotherapy and chemotherapy directly below, including the different combinations of immunotherapy and chemotherapy drugs your doctor may recommend for you.
Immunotherapy drugs
Immunotherapy drugs stick to lymphoma cells and help your immune system find and destroy them. The most common immunotherapy drugs used to treat follicular lymphoma are called rituximab and obinutuzumab.
Rituximab and obinutuzumab are types of monoclonal antibodies, which means they target a specific protein on the surface of lymphoma cells. This helps your immune system to find and kill the right cells, and minimizes damage to your healthy cells.
Some people may be given rituximab on its own, without any chemotherapy drugs, as it can be an effective treatment by itself in some cases. This is called single line immunotherapy.
Chemotherapy drugs
Chemotherapy drugs work by stopping lymphoma cells from growing and dividing. Most people will have a single chemotherapy drug called bendamustine alongside an immunotherapy drug – either rituximab or obinutuzumab. This is sometimes referred to as R-bendamustine or O-bendamustine.
Other people will need to have a combination of different chemotherapy drugs with either rituximab or obinutuzumab as well.
The most common combination of chemotherapy drugs for treating follicular lymphoma is called CVP. Other people may have a slightly different combination called CHOP. This is why you might hear your treatment referred to as R-CVP or R-CHOP. The letters stand for the initials of the immunotherapy and chemotherapy drugs involved, as well as a steroid.
R-CVP (or O-CVP)
- R – rituximab, or O – obinutuzumab, a monoclonal antibody and type of immunotherapy drug
- C – cyclophosphamide, a chemotherapy drug
- V – vincristine, a chemotherapy drug (also known as oncovin)
- P – prednisolone, a steroid that helps to treat the lymphoma and can also help to reduce any inflammation (swelling) and stop you feeling sick.
R-CHOP (or O-CHOP)
- R – rituximab, or O – obinutuzumab, a monoclonal antibody and type of immunotherapy drug
- C – cyclophosphamide, a chemotherapy drug
- H – doxorubicin, also known as hydroxydaunorubicin, a chemotherapy drug
- O – vincristine, a chemotherapy drug (also known as oncovin)
- P – prednisolone, a steroid that helps to treat the lymphoma and can also help to reduce any inflammation (swelling) and stop you feeling sick.
Lots of people are nervous about having chemo-immunotherapy, and the warnings on the drug leaflets can be scary if you weren’t expecting to see them. Ask your doctor or nurse to explain more about how the drugs work and how they may affect you, and contact us if you want to talk about anything.
If you’re worried about side effects, ask your hospital team if there’s anything they can suggest that might help.
"I heard so many horror stories about treatment, and people being totally floored by it. I expected the worst, but in the end it wasn't so bad after all. I got used to it."
Allison, living with follicular lymphoma since 2021. Read more real stories from people affected by blood cancer.

Radiotherapy
Radiotherapy is a common treatment for people with early stage follicular lymphoma, and can be very successful by itself. Others with more advanced follicular lymphoma might need to have a course of radiotherapy as well as chemo-immunotherapy.
Radiotherapy works by targeting a particular area of your body with radiation using a machine, so your doctor may recommend it if you only have one lump, or if the lymph nodes affected by the lymphoma are all in the same place. It can also help with symptoms such as pain or irritation caused by the location of any lumps or swelling.
It’s worth knowing that radiotherapy can irritate your skin, and sometimes results in scarring. Ask your hospital team if there's anything you can do that might help prevent this. You can also read our information about itching which contains hints and tips on how to cope with skin problems.
How will I have treatment?
Treatment is usually given in cycles, which is a period of treatment followed by a period of rest to allow your body to recover. Your doctor or nurse will tell you how many cycles they’ll think you need in a round of treatment.
Most people will go to the hospital or a clinic as an outpatient to receive their treatment. If you’re having chemo-immunotherapy, each cycle can involve travelling between the treatment centre and your home multiple times per week for many weeks in a row. Your appointments will usually take around 2-3 hours each, but your first one may take longer as your nurse will introduce the drugs slowly to help prevent a reaction.
If you’re having radiotherapy, your treatment course will be shorter, but you’ll still have to travel to the hospital and back every day for a few days in a row, over a period of weeks. The radiotherapy itself will only take a few minutes each time, but there may be a lot of waiting around before it’s your turn.
It’s worth knowing that if you are having a combination of treatments you might have to visit different hospitals on a regular basis, as not every hospital offers every type of treatment.
Coping during treatment
As well as dealing with side effects, many people find that having treatment is stressful and disruptive to your life. This can be especially frustrating if you’re usually a very busy person or have others depending on you. Don’t be afraid to speak to your doctor about how treatment may affect you and your routine, and ask if there’s any support you can access. You might also want to consider whether there’s anyone you know that could help out when needed, such as giving you a lift to your appointments, cooking you meals, or looking after children or pets.
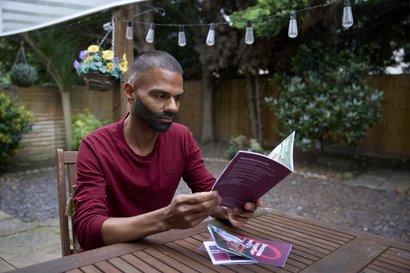
We have more information about the impact of treatment and how to cope during treatment in our printed booklet about follicular lymphoma – download it from our online shop or order a printed copy for free.
"You just have to find something works for you. I think of follicular lymphoma as one chapter in my life. I have other things going on, other chapters as well. That helps me deal with it."
Sarah, living with follicular lymphoma since 2023. Read more real stories from people affected by blood cancer.

Maintenance therapy
After you’ve finished a round of treatment, you may be offered maintenance therapy. This aims to stop the lymphoma coming back for as long as possible.
Maintenance therapy normally involves treatment with an immunotherapy drug such as rituximab or obinutuzumab. You’ll need to go to the hospital once every couple of months for around two years, and it's usually given through a vein in your arm (an IV drip) or via an injection under your skin.
Second line treatment
If the first course of treatment you have doesn’t work, or if the follicular lymphoma comes back later on, you might need to have more treatment. This is called second line treatment.
You might also need second line treatment if you have refractory or transformed follicular lymphoma.
Your doctor will look at how well your first round of treatment worked, how long it’s been since you had treatment, and where any new lumps have appeared when deciding which second line treatment to recommend.
Second line treatment options include:
- the same combination of chemo-immunotherapy drugs you tried last time, in a higher dose
- a different combination of chemo-immunotherapy drugs
- an immunotherapy drug on its own (single line immunotherapy)
- joining a clinical trial
- more intensive treatment, such as a stem cell transplant.
Your hospital team will be able to tell you more about second line treatment and which options may be suitable for you.
If you join a clinical trial, you may be able to try a new drug or a new combination of drugs that are not otherwise available. Find out more about trials on our clinical trials page, or call our Clinical Trials Support Service on 0808 2080 888.
Why can't the lumps just be removed?
If you have swollen lymph nodes, you might wonder why the lumps can’t be removed in one go like with solid tumours such as breast cancer. This is because lymphoma cells (called B lymphocytes) can go wherever your blood goes. B lymphocytes can then gather together, creating lumps which may be found all over your lymphatic system. This includes areas deep inside your body where you may not be able to see or feel them.
Without the right kind of treatment, the B lymphocytes would just keep growing and travelling around your lymphatic system, and more lumps would appear. Treatment for follicular lymphoma therefore targets the whole lymphatic system, not just the specific area where the lump is.
Order printed health information
Our blood cancer information is written with expert medical professionals and people affected by blood cancer. Our information booklets cover many different types of blood cancer and topics, including information for people newly diagnosed.
More About This