Research impact on lymphoma
Our research in lymphoma has focused on improving treatments.
Understanding the causes of lymphoma
In 1998, the Blood Cancer UK-funded Epidemiology and Cancer Statistics Group (ECSG) began a study to investigate the possible causes of Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). The study looked at the following factors: family history and other genetic factors, lifestyle factors such as smoking, alcohol and obesity, and illnesses and health events that precede a diagnosis of lymphoma.
The study has provided evidence that indicates that infections do not increase the risk of getting NHL, and that postmenopausal hormone therapy decreases the risk of NHL by around 30%.
It has also indicated that hormonal contraception is associated with a 30% increased risk of follicular lymphoma, but that there is no increase in the risk of diffuse large B-cell lymphoma (DLBCL).
Improving the diagnosis of lymphoma
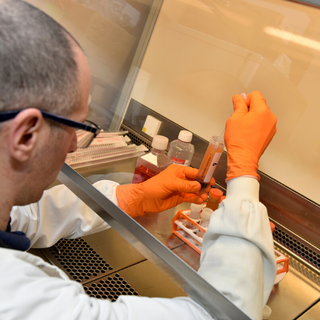
Research that we funded since the 1980s has transformed the diagnosis of lymphoma. We funded Professor David Mason between 1976 and 1986 who developed several methods for using antibodies (molecules which stick to cancer cells) to diagnose lymphoma.
Professor Mason developed an antibody against the anaplastic large cell lymphoma (ALCL) protein, called ALK1. His discovery has improved the diagnosis and management of ALCL that was previously difficult to diagnose, and which caused delays in treatment.
Mason also helped to pioneer a new way of naming molecules on the surface of white blood cells. He was one of the most enthusiastic promoters and organisers of meetings on human leukocyte differentiation antigens (HLDAs) that led to the introduction of a new classification system called ‘cluster of differentiation’ (CD). If you look at any of the new antibody-based drugs available today, many target different ‘CD’ molecules, named using the system that Professor Mason developed.
Professor Mason’s work at Oxford University was continued by Professor Alison Banham, with funding from us. She also made a major contribution in improving the diagnosis of lymphoma.
Making Hodgkin lymphoma treatment kinder
We funded the RAPID trial, which looked into the treatment of Hodgkin lymphoma. This trial was led by world-renowned lymphoma specialist, Professor John Radford, at The Christie in Manchester. Before the RAPID trial, people with Hodgkin lymphoma did not get positron emission tomography (PET) scans before treatment. Instead, they would undergo one PET scan at the end of treatment. Everyone with early stage Hodgkin lymphoma was treated with chemotherapy and radiotherapy.
The RAPID trial was designed to test whether PET scanning could be used to determine if a patient needs radiotherapy. The trial tested whether chemotherapy alone would be sufficient in those patients who have a negative PET scan after three cycles of chemotherapy. RAPID showed that people who had a clear PET scan after chemotherapy had a very good outcome without having radiotherapy. This is important because less intensive treatment means patients experience fewer side effects, which can include secondary cancers and heart disease.
This research has changed clinical practice worldwide.
Improving treatment in hard-to-treat lymphomas
We’ve invested nearly £3 million in the Precision Medicine in Aggressive Lymphoma (PMAL) consortium. PMAL is a team of researchers based in the UK, comprised of clinicians, bioinformaticians, and lab-based researchers. Together, they are working on gaining a deeper understanding of the genetics behind different kinds of lymphoma and how those genetics can differ from person to person. This means doctors can match the right treatment to each individual.
The first clinical trial from PMAL was REMoDL-B and was led by Professor Peter Johnson and Professor Andy Davies at Southampton University. This proved it was possible to use tests to look at the different levels of genes in lymphoma samples. The test results would then be used to group people for treatments, giving people the most appropriate treatment for their disease. As a result of this investment, the PMAL team has already established a new classification system for aggressive lymphoma.