Blood Cancer UK funding led to understanding the origins of childhood leukaemia in twins
New research has shed light on the origins on a type of blood cancer – childhood acute lymphoblastic leukaemia – and how it develops in children.

Researchers at the Institute of Cancer Research (ICR) confirmed this cancer originates in the womb but that events after birth determine whether or not leukaemia develops. The scientific journal, Leukemia, published the results of the first-of-its-kind study.
What did the researchers find?
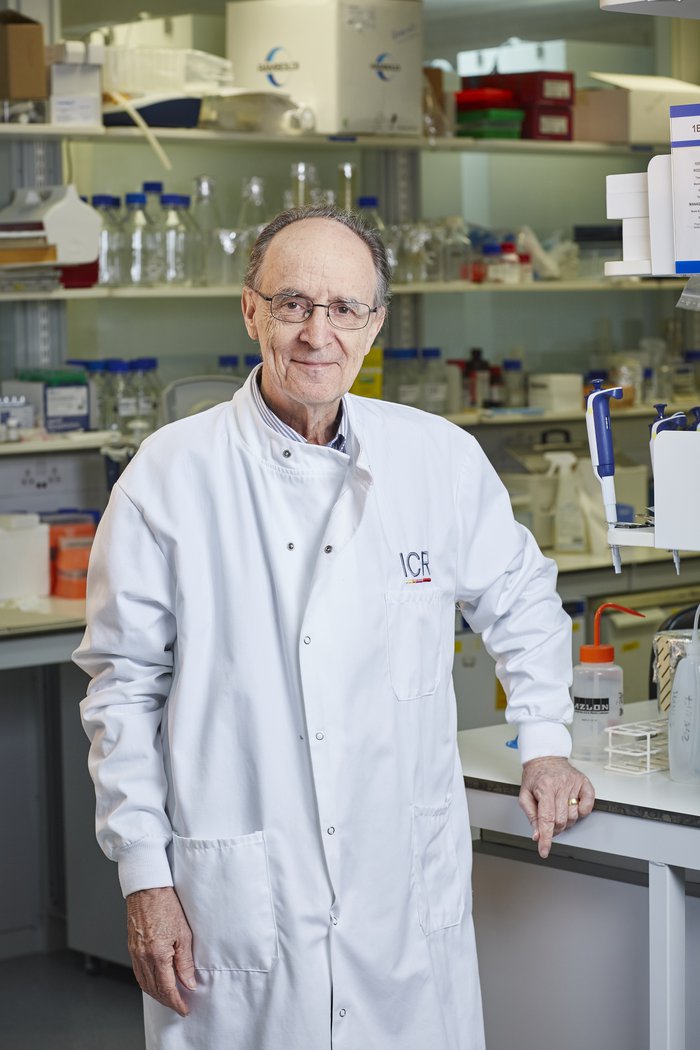
Acute lymphoblastic leukaemia (ALL) is the most common type of childhood cancer in the UK. To find out more about the disease, Professor Sir Mel Greaves and his team studied leukaemia in identical twins for 15 years.
Their research found that if one twin develops leukaemia, the other twin has a higher risk of also developing the disease.
This is because two changes are needed to determine whether a child develops leukaemia. One change before birth, which both children will have if they’ve shared a blood supply, and one after. The researchers think that this is caused by an event like an infection and may only affect one sibling.
In cases where both twins shared a placenta, their twin sibling will also have this first change and could be closely monitored. If it looks like they are going to develop leukaemia, they could be treated early, giving them the best possible chance of survival.
This research could also mean better advice to families who have twins affected by leukaemia.
Sarah McDonald, Deputy Director of Research, at Blood Cancer UK, said:
“Acute lymphoblastic leukaemia (ALL) is the most common type of cancer in children, affecting children more often than adults.
“Understanding the mechanism as to how the cancer develops in identical twins, and why often only one develops leukaemia is an important question to answer.
“It helps us understand both the risk of the remaining twin developing leukaemia and provides insight into how leukaemia develops in all children.”
Speaking about his team’s work, Professor Sir Greaves at the ICR, who conducted the research said:
“What remained a mystery until now was why sometimes only one twin is diagnosed with leukaemia – leaving clinicians in the dark when it comes to offering advice and reassurance to parents.
“In this new study, we show that the healthy twin often has a small number of pre-leukaemia cells in their blood, which have the same genetic markers as the cancer cells in the sick twin."
What do the findings mean for the blood cancer community?
The new findings suggest that the risk of the healthy twin developing leukaemia could be more accurately assessed – firstly by determining whether the twins are identical and shared a placenta and then by tracking the levels of cell that could lead to leukaemia [RK3] in their blood.
If the levels of these cells were to go up and it looked like the healthy twin was going to develop leukaemia, treatment could start at an early stage, giving them the best possible chance of survival.
The findings could help clinicians advise parents of twin children with ALL, offering guidance on risk level and screening. In the past, parents have been given variable advise on risk to any healthy twin when the other develops the disease.
Speaking about the impact of the work, Blood Cancer UK’s Sarah McDonald said:
“This research shows that in cases where one twin develops leukaemia, and both twins both share a placenta during pregnancy, two events are needed to determine whether the sibling develops the disease - one before birth and the other after.
"This work, made possible by research volunteers with leukaemia over a number of years, opens up the possibility of seeing if the unaffected sibling has pre-leukaemia cells in their blood. If they do, it may mean that they can be closely monitored and treated early if it looked like they were going to develop leukaemia, giving them the best possible chance of survival. This finding could also help clinicians give guidance to families on the likelihood of the sibling developing childhood ALL.
“On behalf of Blood Cancer UK, we want to thank our supporters, who enable us to fund pioneering research like this. While this research adds to our understanding about how childhood ALL is triggered, there’s still more to be done to complete the picture, to get to the days where no lives are lost to blood cancer.”

Fund blood cancer research
The day we beat blood cancer is now in sight, but we need your help to get there.